Diabetes Mellitus is categorized by disorders of carbohydrate, protein and fat metabolism. Diagnostic tests are numerous, most of them are given below
Urine “Glucose”
– lacks sensitivity = positivity in disease
– poor specificity = negativity in health
• Problems
– renal threshold variable 6 to 15 mmol/L
– interferences : Clinitest / Glucose oxidase strips
If urine test positive a confirmatory blood test is needed
Blood Tests
• Glucose
– whole blood 10-15% lower than plasma
– venous 10% lower than capillary
– Preservatives not 100% effective
• heparin / serum – loss of 1 mmol/L per 2 hours
• fluoride / oxalate – loss of about 10% overnight
• Insulin / glycosylated Hb / fructosamine
– No use for diagnosis
Diagnostic Criteria
• Plasma glucose :
A) Symptoms + random value > 11.1 mmol/L
B) Fasting value > 7.0 mmol/L
C) 2-h post glucose load (75g) value > 11.1 mmol/L
If one of these criteria is met then repeat testing the following day is required for confirmation
Oral Glucose Tolerance Test (OGTT)
• Complicated test no longer recommended for routine use except in pregnancy
• Still available in many laboratories
• Still found in text books
• Used in testing in pregnancy
• This evaluates the endogenous insulin response to a physiological glucose challenge
• The diagnostic value of OGTT has been over estimated and is used too frequently in situations where it is not needed
• In the absence of a specific marker of the diabetic state the OGTT remains the most sensitive and practical test for the early recognition of asymptomatic diabetes, without fasting hyperglycaemia even if it is a non-specific test.
Indications of OGTT
• Evaluation of a person with a borderline elevation of fasting or post prandial plasma glucose
• Diagnosis of gestational D.M
• High risk individuals
• Evaluation of glycosuria
• Assessment of unexplained presence of what might be expected a diabetic complication e.g. Neuropahty
• Metabolic condition (elevated triglycerides)
• Obesity
• Clinical or epidemiological research projects
Preparation Of Patient For OGTT
• The patient must be ambulatory and free from pyrexia, acute illness or trauma for at least two weeks.
• He/she should have diet containing at least 150 g carbohyrate per day for three days prior to test
• Any drug that alter blood glucose level should also be discontinued prior to testing for 03 days.
• The test should be done in the morning
• The patient must have 8 – 16 h fast.
• Heavy tea and coffee drinkers should reduce their consumption
• Smoking should be avoided
• No physical exercise or activity is allowed
• Patient should be seated quietly and relaxed for 30 minute for test
Procedure For OGTT
• Glucose load
– For adults 75 g glucose
– For children 1.75 g/kg body weight
– Glucose load is given in water (25 g/dl)
• This blood samples are taken at half hourly interval up to 2 hours
• Urine samples are usually not required for the diagnosis of diabetes mellitus
Interpretation Of OGTT
• Normal
– Fasting < 5.5 mmol/l
– 0.5, 1.0, 1.5 hrs < 10 mmol/l
– 2 hrs sample < 7.8 mmol/l
• Diabetic
– Fasting > 7.8 mmol/l
– 2 hours or one intermediate
– Sample > 11.1 mmol/l
• Impaired OGTT
– Fasting < 5.5-7.8 mmol/l
– One intermediate sample > 11.1 mmol/l
– 2 hrs between 7.8 and 11.1 mmol/l
OGTT In Gestational D.M
• OGTT is done with a glucose load of 100g
• Blood samples are taken up to 3 hrs, at least two values must exceed the following
fasting 5.8 mmol/l
1 hr 10.5 mmol/l
2 hrs 8.6 mmol/l
3 hrs 7.8 mmol/l
Fasting Plasma Glucose
• Reference range for plasma glucose for venous blood sample (3.3-5.5 mmol/l) – 60-100 mg/dl
• Duration of fast 10-14 hrs
• It is a specific screening test
• Glucose value > 7.8 mmol/l (140 mg/dl) is diagnostic
• Precautions
– Normal diet (carbohydrate 150g/day)
– Absence of diseases which are known to cause hyperglycemia
• Limitations
– Fasting hyperglycemia occurs relatively late in some patients of NIDDM
• Post challenge plasma glucose/OGTT is suggested when fasting glucose is between 5.5-7.8 mmol/l.
• Note: after 50 yrs of age; add 0.6 mmol per decade or 1 mg/year to the diagnostic criteria
Random Plasma Glucose
• In healthy individuals, plasma glucose conc. Vary only slightly throughout the day and generally are in the range of 2.5-7.3 mmol/l. The only rise that occurs is found following a meal.
• Diagnostic value
– > 11.1 mmol/l – dm
– < 2.5 mmol/l hypoglycaemia 7.8-11.1 mmol/l
– Further investigations
• Random glucose has no value in screening, diagnosis and follow up of DM
• It has greatest value in comatosed patients, whether known or preveiously unknown diabetes.
Post Challenge Plasma Glucose
• Glucose load = 75 g
• Plasma glucose conc. Is determined 2 hrs later
• It allows for more objective conditions of testing and a more precise comparison of an individual’s response with a large population. This test is more precise than a postraprandial glucose
• However this test requires more preparation
• Unrestricted activity
• Carbohydrate diet
• Fasting
• Diagnostic value – 11.1 mmol/l
Two Hour Postprandial Plasma Glucose
It has been used to screen for diabetes mell-itus, to diagnose diabetes and to monitor glucose control. The significance of the 2 hrs postprandial value is limited by the lack of rigidly controlled conditions
• Amount of carbohydrate
• Time used to consume meals
• Type of food
• Age of the patient
• Time of the day
These factors are responsible for the differences in the interpretation of the results
• Interpretation:
– Glucose value < 7.8 mmol/l normal
– Glucose value 7.8 – 11.1 mmol/l ogtt
– Glucose value >11.1 mmol/l dm
Sampling For Blood Glucose
A. Whole blood allowed to stand at room temperature shows decrease in glucose from 7-10% in one hour
• The erythrocytes of newborn infants consume glucose more rapidly (20-30%/hrs)
• Procedures for the prevention of glycolysis in blood specimens should be adopted to prevent decrease in glucose before estimation
B. Venous/capillary blood
C. Plasma/whole blood
• It provides more stable values for glucose
• No effect of hematocrit
• It reflects the extracellular glucose concentration more accurately
Conclusions
• Fasting plasma glucose can be offered as a single screening test
• The patients having fasting glucose level between 5.5 – 7.8 mmol/ can be further evaluated with either post challenge glucose or OGTT
• Random glucose should only be reserved for patient presenting as medical emergency
• 1 mg/dl per year of age (0.6 mmol/decade)after the age of 50 years must be added to the accepted normal range of glucose for correct interpretation of the results.
Looking for complications
Need to monitor for long-term complications – biochemistry is useful as a screen
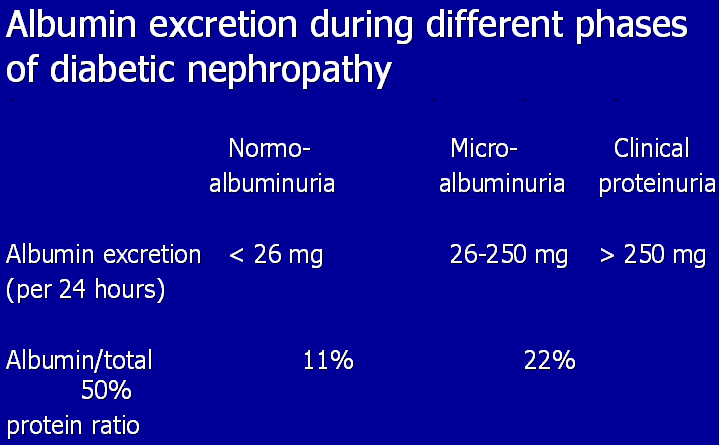
– Renal
• Plasma creatinine (50-140 µmol/l)
• Urine “microalbumin”
• < 30 µg/min in resting overnight sample
– Lipids
• Fasting triglycerides (< 1.7 mmol/l)
• Cholesterol (< 5.1 mmol/l)
– ? Thyroid function tests
• Autoimmune association IDDM
• May be justified especially in elderly females
Acute events
Diabetic Ketoacidosis
• Caused by insulin deficiency and often precipitated by intercurrent illness
• increased glucagon, cortisol, catecholamines, GH causes increased hepatic glycogenolysis & gluconeogenesis and unrestrained FFA release from adipose tissue
• beta-oxidation in liver produces excess ketone bodies causing acidosis
• dehydration due to osmotic diuresis leads to renal impairment and failure to compensate for acidosis
• Usually a long prodromal period followed by a rapid onset of acidosis and catastrophic collapse
DKA – Biochemistry
• Severe Acidaemia & Acidosis
– pH may be 6.75 – 6.9 (ref 7.35 – 7.45)
– Kussmaul breathing
• Hyperglycaemia
• Hyperkalaemia
– H+ exchange across membranes for K+
– but note this masks a severe intracellular K+ deficiency
DKA -diagnostic testing
• Clinician – at bedside
– test strip blood glucose
– arterial blood pH, pO2, pCO2
• Laboratory
– confirms glucose
– plasma U&E (creatinine unreliable)
• low sodium
– may be due to glucose osmotic dilution
– may be pseudo due to hyperlipidaemia
• high potassium
– due to acidosis
Hypoglycemic Coma
Symptoms : coma, tachycardia, sweating, fits
• Immediately test strip glucose
– beware credibility of low results
– and failure to diagnose
• Treat if in any doubt – glucose is harmless!
• Confirm with lab blood/plasma glucose BUT take sample before treatment
– blood glucose < 2.2 mmol/L
– plasma glucose < 2.5 mmol/L
Hyperosmolar Hyperglycaemic coma (HONK)
• Elderly NIDDM
– some mild ketosis, lack of hyperventilation
– 50% raised plasma Na > 150mmol/L
– glucose typically 50 – 60 mmol/L
• 50% mortality – widespread venous thrombosis
• Good prognosis if well managed
Want a clearer concept, also see
 howMed Know Yourself
howMed Know Yourself


Thanks for the work well presented. My questions and uncertainities got cleared by the straight forward and well organised information. My academic challenge questions found an applicable quide.