Family planning is a way of thinking & living that is adopted voluntarily, upon the basis of knowledge, attitudes & responsible decisions by individuals & couples, in order to promote the health & welfare of the family group & thus contribute effectively to the social development of a country.
Objectives
- To avoid unwanted births.
- To bring about wanted births.
- To regulate the intervals between pregnancies.
- To control time of births in relation to the ages of the parents.
- To determine the number of children in the family.
Scope of Family Planning Services
It includes:
- The proper spacing & limitations of births.
- Advice on sterility
- Sex education.
- Education for parenthood
- Screening for pathological conditions related to the reproductive system
- Genetic counseling
- Premarital consultation & examination.
- Carrying out pregnancy tests.
- Marriage counseling.
- Preparation of couples for the arrival of their 1st child.
- Providing services for single / unmarried mothers.
- Teaching home economics & nutrition.
- Providing adoption services
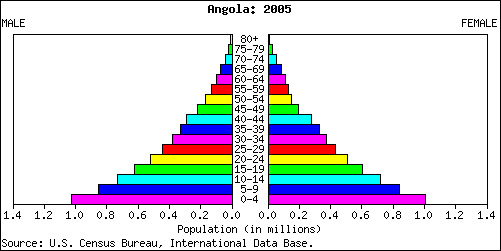
Eligible Couples
An eligible couple is a married couple where the age of the wife is between 15-45 years. There are 100-120 such couples per 1000 population. About 20% of eligible couples are found in the age group 15-24 years. Approximately 1.5 million couples are joining the reproductive group each year.
These couples are in need of family planning services.
Target Couples
These are couples who are a priority group & who already have 2-3 living children.
Couple Protection Rate
It is an indicator of the prevalence of contraceptive practice in the community. It is defined as the percentage of eligible couples effectively protected against childbirth by one of the approved methods of family planning, which are sterilization, IUD, condom or oral pills, etc.
Health Aspects of Family Planning
Health aspects of family planning include:
1. Women’s health
It occurs primarily through:
- Avoidance of unwanted pregnancies.
- Limiting & spacing births.
- Timing the 1st & last birth according to mother’s age.
- Reducing maternal mortality & morbidity.
- Improving nutritional status
- Preventing complications of pregnancy & abortion.
2. Fetal health
Fetal health by reducing fetal mortality and abnormal Development
3. Infant & child health
Infant and child health by reducing neonatal, infant & preschool mortality and determining health of the infant at birth as well as vulnerability to diseases.
An ideal contraceptive must be:
· Safe
· Effective
· Acceptable
· Inexpensive
· Reversible
· Simple to administer
· Requiring little or no medical supervision.
· Long lasting
Methods of Contraception
Temporary or Spacing Methods:
Barrier methods:
Physical methods
Chemical Methods
Combined Methods
Intra-uterine devices
Hormonal methods
Post-conceptional methods
Miscellaneous
Permanent Methods:
In the Female: Tubal ligation
In the Male: Vasectomy
Barrier methods
Physical methods
Condoms:
- Male Condoms
- Female Condoms
Diaphragm
Vaginal Sponge
Barrier methods advantages:
· No Side Effects
· Protection from STD’s
· Protection from PID’s
· Protection from Cervical Cancer
Disadvantages:
· Requires high degree of Motivation
· Less Effective than the Pill or IUCD’s
Chemical Methods
Mechanism of action:
These are “surface- active agents” which attach themselves to the spermatozoa & inhibit oxygen uptake and kill sperms.
These are divided into 4 categories:
1. Foams: tablets, aerosols
2. Creams, jellies & pastes
3. Suppositories
4. Soluble films
Intra Uterine Contraceptive Devices
Basic Principle
The control of conception by introduction of a foreign body into the uterus. Today, 65 million women use some type of IUCD for contraception.
Types of IUCD’s
Non-medicated :
First Generation IUCD’s
Medicated:
Second generation (copper)
Third generation (hormone releasing)
Mechanism of Action Of IUCD’s
The foreign body reaction in the uterus causes cellular & bio chemical changes in the endometrium & uterine fluids. These changes impair the viability of the gamete thereby reducing its chances of fertilization. Medicated IUCD’s by releasing copper increase the cellular responses & enzymes in the uterus. Copper ions alter the biochemical composition of the cervical mucosa affect sperm motility, capacitation & survival.
Hormone releasing devices increase the viscosity of the cervical mucosa & thereby prevent sperm from entering the cervix. High levels of progesterone & low levels of oestrogen sustain an unfavourable endometrium.
First Generation IUCD’s
These are the inert or non-medicated devices made of polyethylene or other polymers. They are available in different shapes & sizes, e.g. coils, spirals, loops, rings, etc.
Lippes Loop
A double S-shaped spiral device made of non-toxic, non-tissue reactive & durable material. It contains a small amount of Barium Sulfate. Attached thread projects in the vagina, so that it reassures the user that the loop is in place & also for easy removal purposes.
Second Generation IUCD’s
With the addition of copper; medicated & second generation IUCD’s came into existence.
EXAMPLE: Copper-T or Multiload
Advantages:
- Effective life of at least 5 years.
- Low expulsion rates.
- Lower incidence of side-effects,eg. pain & bleeding.
- Easier to fit even in nulliparous.
- Increased contraceptive effectiveness
Third Generation IUCD’S
Progestasert
T-Shaped device filled with progesterone. Hormone is released slowly in the uterus @ 65mcg/day. It has direct local effect on uterus lining, cervical mucosa & sperms.
Levonorgestrel
T-Shaped device releasing synthetic steroids @ 20mcg/day. It is associated with less menstrual blood loss and is effective life about 5 years.
The disadvantage is that it is expensive.
Advantages of IUCD’s
- Simplicity &Effective
- Insertion takes a few minutes
- Inexpensive
- Reversible
- Free of systemic metabolic effects
- No continuous motivation required.
Disadvantage:
Mennorhagia and/or Dysmenorrhea.
Contra Indications
Absolute:
· Suspected Pregnancy
· PID
· Undiagnosed vaginal bleeding.
· Cancer of uterus or adenexa & other pelvic tumor.
· Previous h/o Ectopic Pregnancy.
Relative:
· Anemia & Menorrhagia
· History of PID
· Purulent cervical discharge.
· Fibroids in uterine cavity.
Side Effects & Complications of IUCD’S
· Bleeding
· Pain
· Pelvic infection
· Uterine perforation
· Pregnancy
· Ectopic pregnancy
· Expulsion
Ideal IUCD Candidate
1. Woman who has born at least one baby
2. No h/o PID
3. Has a normal menstrual cycle
4. Is willing to check the IUCD tail
5. Has access to regular follow-ups & treatment of potential problems.
Timing of Insertion of IUCD’s
· During menstruation or within 10 days of the beginning of the period.
· Within the 1st week after delivery
· 6-8 weeks after delivery.
Follow- Up
It is very important to provide motivation & emotional support. It is also important to confirm the presence of the IUCD and diagnose or treat any side-effect or complications.
Instructions to regularly check the threads, & if unable to do so, must consult the doctor immediately are also given. The woman is told to report any side effects & complications and to consult a doctor if she misses a period.
Hormonal Contraceptives
They act by stopping ovulation from taking place. Combined oral contraceptives when properly used, are almost 100% effective in preventing pregnancy.
Gonadal steroids
Synthetic oestrogens:
Ethinyl oestradiol
Mestranol
Synthetic Progestogens
Preganes
Oestranes
Gonanes
All are converted to norethisterone before becoming active. Gonanes are the best tolerated,e.g. Levonorgestrel.
Classification
Oral Pills
· Combined pill
· Progestogen only pill
· Post coital pill
· Once-a-month pill (long acting)
· Male pill
Depot (Slow Release) Formulations
· Injectables
· Subcutaneous implants
· Vaginal rings
 Combined Oral Pills (COC)
Combined Oral Pills (COC)
It is a major spacing method of contraception. Most formulations contain 30-35 mcg of a synthetic estrogen & 0.5-1 mg of Progestogen.
Dosage: one pill for 21 consecutive days, starting from 5th day of period, followed by a break of 7 days- when periods occur.
Pill must be taken daily at a fixed time. If missed, then should administer it as soon as possible & next pill should be taken at usual time.
Oral Pills
Mode of Action
Prevent the release of the ovum from the ovary by blocking the pituitary secretion of gonadotrophins, necessary for ovulation to occur. Progestogen only pills make cervical mucus thick & scanty thereby inhibiting sperm penetration.
Progestogens also inhibit tubal motility & delay the transport of sperm & ovum to the uterine cavity.
Actions of COC’S
· Inhibit ovulation
· Inhibit implantation of the zygote
· Accelerate ovum transportation
· Make the cervical mucosa thick & cellular
· Inhibit sperm capacitation
· Offer reversible contraception.
Progestogen Only Pill
Contains only progestogen which is released in small doses throughout the cycle.
Advantages:
In older women, in whom COC are contraindicated due to cardiovascular risks progestogen only pills may be given. Younger women with risk factors for neoplasia may also benefit from these.
Disadvantage:
Poor cycle control and increased pregnancy rate.
Post Coital Contraception
It is recommended within 48 hours of unprotected intercourse. It is advised as an emergency method, after rape or contraceptive failure.
An IUCD can be inserted within 7 days if acceptable. (Cu T)
COC in a double dose is preferred. 2 pills immediately followed by 2 more after 12 hours.e.g. Postinor, Emkit
Once a Month (long acting) Pill
A combination of long acting estrogen and short acting progestogen. Pregnancy rate too high with this and bleeding irregular.
Male Pill –Gossy Pol
Contra Indications of Oral Pills
Absolute
· Cancer of the breast and genitals
· Liver disease
· Previous and present history of thromboembolism.
· Cardiac abnormalities
· Congenital hyperlipidemia
· Undiagnosed abnormal uterine bleeding
Special Problems Requiring Medical Surveillance
· Age over 40 years
· Smoking and age over 35 years
· Mild hypertension
· Chronic renal disease
· Epilepsy
· Gallbladder disease
· Nursing mothers (in 1st 6 months)
· Diabetes Mellitus
Danger Signs of Pill Use
· Severe abdominal pain
· Chest pain with cough and shortness of breath
· Severe headache, dizziness, weakness or numbness
· Eye problems (vision loss or blurring)
· Speech problems
· Severe leg pain (calf & thigh)
Adverse Effects of Oral Pills
CARDIOVASCULAR EFFECTS
Myocardial infarction
Cerebral thrombosis
Venous thrombosis
Hypertension
CARCINOGENSIS
Cervical cancer with increased duration of use of COC.
METABOLIC EFFECTS
Altered serum lipids
Blood clotting
Liver disorders
Carbohydrate metabolism.
Oral pills common unwanted side effects
· Breast tenderness
· Weight gain
· Headache and migraine
· Bleeding disturbances
Oral Pills Beneficial Effects
Almost 99-100 % contraceptive effectiveness. Give protection against :
· Benign breast disorders
· Ovarian cyst
· Iron deficiency Anemia
· Pelvic inflammatory disease
· Ovarian tumor
· Ectopic pregnancy
Depot Formulations
These are highly effective, reversible, long acting and estrogen free with a single administration for several months or years. These include:
1. Injectable contraceptives
DMPA
NET-EN
2. Sub dermal implants:
Norplant
3. Vaginal Rings
DMPA
Depomedroxy Progesterone Acetate or Depo Provera.
A safe, effective & acceptable contraceptive. It does not effect lactation and gives 99 % contraceptive protection.
Mode of action:
· Suppression of Ovulation
· Indirect effect on Endometrium
· Direct action on Fallopian tubes
· Action on the production of cervical mucus.
DPMA
DOSE:
150 mg I/M Injection every 3 months
Side Effects:
· Weight increase
· Irregular menstrual bleeding
· Prolonged infertility
NET-EN
Norethisterone Enantate -Norigest
Mode of action:
· Inhibition of ovulation
· Progestogenic effect on cervical mucosa
DOSE : 200 mg I/M every 60 days.
Administration:
Deep I/M injection during the first 5 days of menstrual period so as to rule out a pregnancy.
Contraindications
· Cancer of the breast
· Genital cancers
· Undiagnosed uterine bleeding
· Suspected malignancy
Subdermal Implants
Norplant
It consists of 6 silicone rubber capsules containing 35 mg each of levonorgestrel. It is implanted subcutaneously in the upper arm. Effective contraception is provided for over 5 years. It is reversible.
Disadvantage:
· Irregular menstrual bleeding.
· Surgical procedure necessary to insert & remove implants.
Miscellaneous (Natural Methods)
- Abstinence
- Coitus Interruptus
- Safe period (calendar method)
- Natural family planning method: a. Basal body temperatureb. Cervical mucus method
- Breast feeding
- Birth control vaccine
- New method, Persona
Terminal methods
Voluntary surgical contraception:
· Male sterilization
· Female sterilization
Advantages:
· One time method
· No sustained motivations required
· Most effective
· Most cost effective
Vasectomy
Procedure:
Under local anesthesia & aseptic precautions, 1cm piece of vas deferens is removed. Ends are ligated & folded back.
Complications:
· Pain
· Hematoma
· Local infection
· Spontaneous re canalization
· Autoimmune response
· Psychological
Tubal ligation
Two procedures are used:
· laparoscopy
· minilap operation
 howMed Know Yourself
howMed Know Yourself