A 25 year old patient was admitted to the emergency department with suspected spinal cord injury[1]. On questioning she gave history of road traffic accident[2]. She told that she was thrown violently forward on impact. She said she could not feel anything in either leg and could not move her legs also. On examination there was complete motor and sensory loss of both legs below the inguinal ligament and absence of all deep tendon reflexes of both legs[3]. Twelve hours later, it was noticed that she could move the toes and ankle of her left lower limb and she had return of sensations of her right leg except for loss of tactile discrimination, vibratory sense and proprioceptive sense. She had a band of complete anesthesia over her right inguinal ligament. Her left leg showed a total analgesia, thermoanaestesia and partial loss of tactile sense. Her right leg was totally paralyzed and the muscles were spastic. The knee jerk was exaggerated and there was right sided Babinski’s response[4]. A lateral radio graph[5] of thoracic part of vertebral column showed fracture dislocation of tenth thoracic vertebrae[6].
Explanation:
[1] Spinal cord injury:
An injury to the spinal cord may cause myelopathy or result in damage to the nerve roots or myelinated fibers or tracts that carry signals to and from the brain.
[2] Road traffic accident:
Road traffic accident is the leading cause of spinal injuries and fracture dislocation of the vertebrae (1/3 of the causes ). Other causes include:
1. Trauma
2. Violence
3. Pathological
4. Infection
[3] Examination at time of admission:
Complete sensory and motor loss below the level of lesion is indicative of spinal shock. The segmental spinal reflexes are depressed due to the removal of influences from the higher centers that are mediated through the corticospinal, reticulospinal, tectospinal, rubrospinal and vestibulospinal tracts. Mostly it persists for less than 24 hours.
[4] Examination after 12 hours:
Loss of tactile discrimination, vibratory sense and proprioceptive sense on right side which are the function of medial leminiscus, which ascend on the ipsilateral side is indicative of right sided hemisection.
Left sided analgesia, thermoanasthesia and partial loss of tactile sense which are the function of anterolateral pathway, ascend contralaterally, as indicated by left sided loss of senses.
Spastic muscles are indicative of motor loss owing to anterior horn damage.
Exaggeration of knee jerk and Babinski response indicates upper motor neuron lesion.
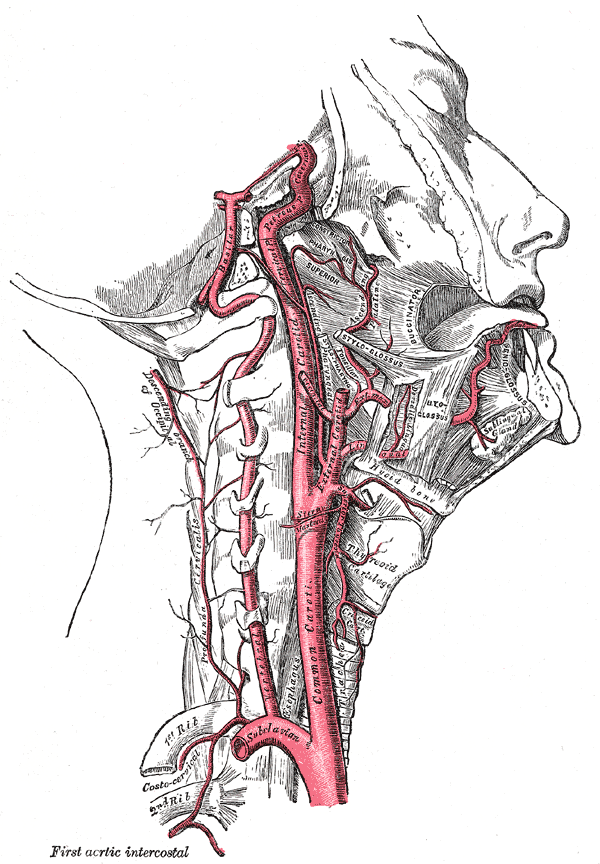
[5] Lab Diagnosis:
Radiograph is commonly used for screening for fractures.
CT scan, as is more sensitive, is used to localize the damage.
MRI is the best option possible available.
[6] Tenth thoracic vertebrae:
Fracture is most common in thoracic region because:
1. Thoracic region is the longest part so naturally has the greatest probability of damage.
2. Spinal canal and vertebral bodies are proportionately smaller
3. Vascular supply is less and there are few collaterals.
Treatment:
a. Stabilization with ABC technique ( Airway, breathing, circulation)
b. Hemodynamic stability
c. Immobilization
d. Operative or non operative treatment.
 howMed Know Yourself
howMed Know Yourself

Meine Zada Acha Prepare kiya hai 😛