•Acute Rheumatic Fever: inflammatory disease with devastating sequelae
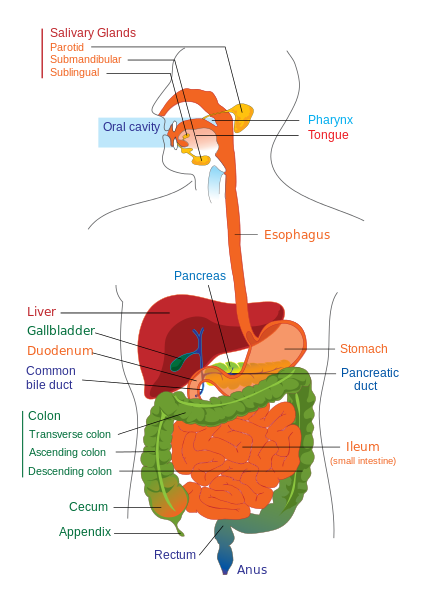
•Link to pharyngeal infection with group A beta hemolytic streptococci
•Continues to be a problem worldwide:
– sporadic outbreaks in developed countries
– frequent occurrences in developing countries
•Best prevention still correct use of antibiotics
Epidemiology
- Estimated 30 million people suffer from ongoing disease from RF, 70% dying at average age of 35 years
- Important cause of chronic disease and death in developing world
- Usually affects people between 5-18 years old
- Males and females affected equally
- Overcrowding, poverty, lack of access to medical care contribute to transmission
- Virulence of strain important
- Antigenic proteins:- M, T, R proteins
Etiology
Beta hemolytic streptococci
Beta hemolytic streptococci
Pathogenesis
•Group A strep pharyngeal infection precedes clinical manifestations of RF by 2-6 weeks
•Antibodies made against group A strep cross react with human tissue:
– heart valve and brain share common antigenic sequences with GAS bacteria
– molecular mimicry
•Host immune responses may determine who gets RF
•Virulent strains: rheumatogenic serotypes
•Perivascular granulmatous reaction – Vasculitis
Clinical Features
•Incubation Period: 2-6 weeks
•Fever( sudden onset), malaise, fatigue
•Arthritis
•Carditis
•Chorea
•Erythema marginatum
•Subcutaneous nodules
•Arthralgias
•Epistaxis
•Serositis
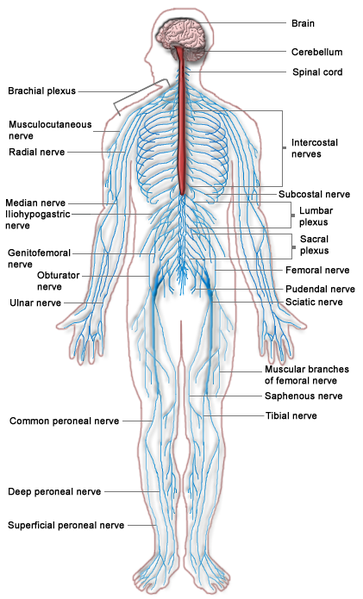
•Involvement of lung, kidneys, CNS
Arthritis
•Most common feature: present in 80% of patients
•Migratory, involves large joints
•Lasts 1-5 weeks and subsides without residual deformity
•Prompt response to therapeutic doses of salicylates or NSAIDS
Carditis
•Most serious manifestation
•May lead to death in acute phase or at later stage
•Any cardiac tissue may be affected:
– Valvular lesion most common
– Seldom see isolated pericarditis or myocarditis
•Signs:
– High pulse rate
– Murmurs
– Cardiomegaly
– Rhythm disturbances
– Pericardial friction rubs
– Cardiac failure
•Mitral(75%) and aortic(30%) regurgitation most common
-Apical systolic and basal murmurs
•Pericarditis usually asymptomatic
-Occasionally causes chest pain, friction rubs or distant heart sounds
Erythema Marginatum
- Seen in upto 7% of patients
- Highly specific to ARF
- Cutaneous lesion:
- Reddish pink border
- Pale center
- Round or irregular shape
- Seen on trunk, abdomen, inner arm or thighs
- Highly suggestive of Carditis
Subcutaneous nodules
•Occur in 9-20% of cases
•0.5-2 cm, firm, non tender, isolated or in clusters along extensor surface of joints(Knees, elbows, wrists)
•Often associated with carditis
Sydenham’s chorea
•Extrapyramidal disorder:
- Fast, clonic, involuntary movements( especially of face and limbs)
- Muscular hypotonia
- Emotional labilty
•Occurs in upto 30% of patients
•½ of those also has carditis or arthritis
•Usually benign and resolves in 2-3 months
•Can last upto 2 years
Diagnosis
Evidence of previous infection with streptococcal upper airway infection and
- 2 major criteria
- 1 major criteria and 2 minor criteria
Diagnosis: Jones Criteria
•Major criteria:
- Arthritis
- Carditis
- Sydenham’s chorea
- Erythema marginatum
- Subcutaneous nodules
•Minor manifestation:
- Fever
- Arthralgia
- Elevated c-reactive protein
- Erythrocyte sedimentation rate
- Prolonged PR interval on EKG
Diagnosis: Evidence of previous infection
Culture
Antistreptolysin antibody
-Often elevated in healthy children or with Rheumatoid Arthritis, Henoch-Shonlein Purpura, Takayasus Arteriti
Differential Diagnosis
•Juvenile Rheumatoid Arthritis
•SLE
•Bacterial Endocarditis
•Reactive Arthritis
Investigations
•Complete Blood Counts
•ESR, C-Reactive Proteins
•ASO Titer
•CXR
•ECG -Prolonged PR interval
•Echocardiography
Treatment
•Eradication of GAS:
Benzathine Penicillin G
- Single dose
- IM
- < 27 years: 600,000 units
- > 27 years: 1200,000 units
•Alternate drugs:
- Penicillin V 500-1000 mg PO divided bid to qid for 10 days
- Erythromycin
- Aaithromycin
- Cephalosporins
Treatment-Arthritis
•Salicylates or NSAIDS for three weeks
•Excellent response
Treatment-Carditis
•Glucocorticoids
•Taper after 2 weeks
Treatment-Chorea
•Haloperidol 0.5-2.5 mg
•Max 5 mg
•Sodium Valproate
Primary Prophylaxis
•Distinguish GAS from Viral Pharyngitis
•Antibiotics
•Improve social and economic factors
Secondary Prophylaxis
•Prevent recurrence of ARF- Benzathine Penicillin G
•Prevention of chronic valve disease
•Newer recommendations: every 2 weeks for 2 years then every 3 weeks •Duration: 10 years or until 21 years old
 howMed Know Yourself
howMed Know Yourself