PRIMORDIAL GERM CELLS
- Gametes are derived from PGCs.
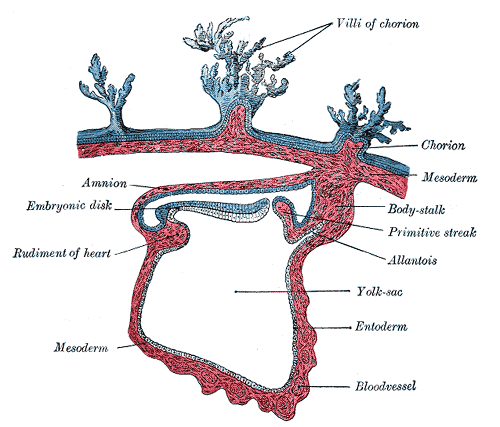
- Formed in the epiblast during 2nd week and move to the wall of yolk sac and reach gonads by end of 5th week
In preparation for fertilization germ cells undergo:
- Gametogenesis
- Cytodifferentiation
OOGENESIS
Is the sequence of events by which germ cells oogonia are transformed into mature oocytes.
OVUM
- Maturation of oocytes begins before birth.
- Accelerates at puberty.
- Ends at menopause.
Morphological changes during maturation of gametes
Maturation of oocytes begin before birth.
A. Primordial germ cell
B. Oogonium
C. Primary oocyte
D. Secondary oocyte
◦By 5th month number of germ cells reaches 7 million in the ovaries.
◦By 7th month majority of oogonia and primary oocyte degenerate.
◦All surviving primary oocytes are surrounded by flat epithelial cells to form primordial follicle
Maturation of oocytes continue at puberty
At birth: Ovaries have about 2 million primordial follicles and all Primary oocytes are arrested in the diplotene stage till puberty due to OMI secreted by follicular cells.
By puberty: Number drops to about 40,000. Rising FSH triggers start of ovarian cycle
Ovarian cycle: Fewer than 500 ovulate in the reproductive life of a female
Recruited Primordial follicle
A. Primordial follicle
B. Growing follicle
C. Primary follicle
Secondary/Antral Follicle
- Longest stage
- Few
- Rapid enlargement
- Stratum granulosum 6-12 cell layers
- Liquor folliculi (hyaluronic acid)
- Formation of antrum
- Oocyte eccentric
- Well defined theca interna & externa
Cumulus oophorus
Is a column of granulosa cells that attaches the oocyte to the follicle wall. At ovulation, this column of cells is broken or separates to release the oocyte from its follicle attachment.
Corona radiata is composed of cumulus cells that send microvilli through zona pellucida that communicate with microvilli of oocyte
Tertiary or Graafian Follicle (Pre ovulatory)
- Spans entire width of cortex & produces a bulge on the surface of ovary
- St. granulosum appears to be thinner
- One large antral cavity
- Cumulus oophorus & corona radiata (loose connection)
- First meiotic division being completed: Primary oocyte divides into a Secondary oocyte and a polar body
Females undergo regular monthly reproductive cycles commencing at puberty.
- Ovarian cycle
- Menstural cycle
Corpus atreticum
Oocytes & its surrounding follicular cells degenerate and replaced by scar tissue.
Ovulation (Release of secondary oocyte)
- Maximum size of follicle
- Sudden surge of LH
- Increase in volume & pressure of follicular fluid
- Overlying ovarian cortex become thin & translucent
- Stigma formation
- Increased collegenase & PG activity
- Increased muscular contractions
Corpus Luteum
- After ovulation, Follicle collapses
- Granulosa and theca interna cells hypertrophy, leutenized & vasularized
- Secretes Progesterone and some estrogens.
Corpus albicans (Absence of HCG)
1.Corpus luteum degenerates and becomes corpus albicans
2.GnRH increases under low estrogen and progesterone levels
OOCYTE TRANSPORT
•Sweeping movements of fimbriae
• Rhythmic contractions
•Motion of cilia
•Fluid currents
Want a clearer concept, also see
Spermatogenesis
 howMed Know Yourself
howMed Know Yourself