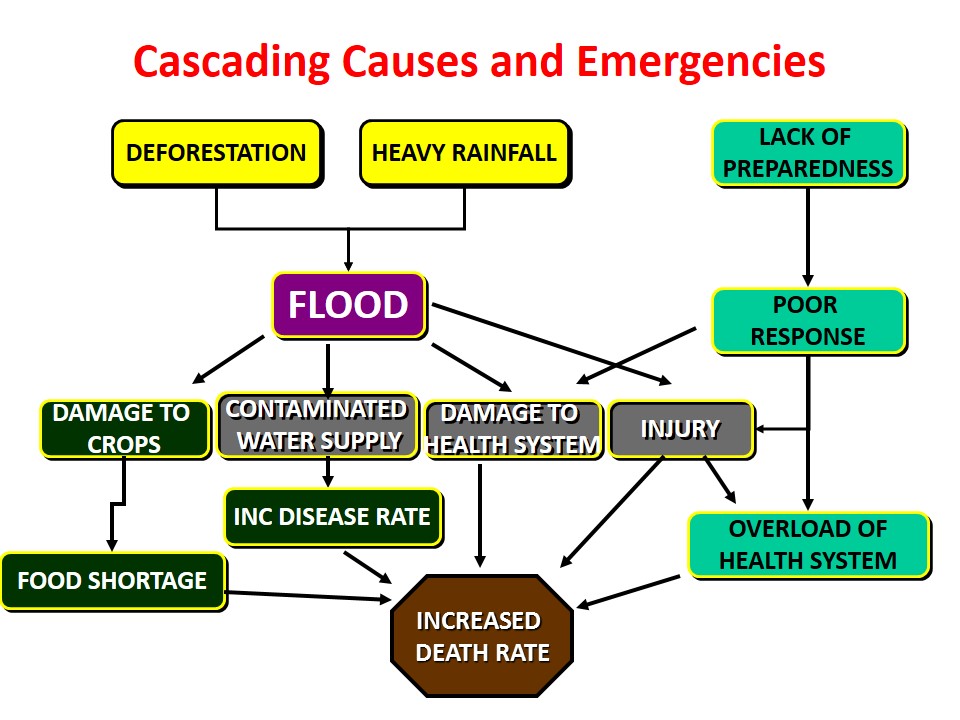
The effects of disasters may be divided into health effects and other effects.
Health Effects
- Injuries & Deaths
- Emotional Stress and Psychological Reactions
- Epidemics
- Increase in indigenous diseases
Other Effects
- Food Shortage
- Disruption of Services / Infrastructure Damage
- Property Damage
- Environmental Damage
Post Disaster Public Health Challenges
Major Public Health Issues (Post disaster)
Environmental pollution
- Water Contamination
- Poor Sanitation
Malnutrition
- Protein Energy Malnutrition (PEM)
- Vitamin A deficiency
Epidemics
- Spread of infectious diseases
Causes of Outbreaks of Infectious Disease in Disasters
- Population displacement
- Environmental changes
- Loss of public utilities
- Disruption of basic health services
- Impact of food scarcity and hunger
Factors for Disease Transmission after a Disaster
- Environmental considerations
- Endemic organisms
- Population characteristics
- Pre- event structure and public health
- Type and magnitude of the disaster
Common Modes of Transmission
Person-to-person
- Measles, Meningitis, ARI
Feco-oral/Enteric
- Shigella, Cholera, Typhoid, Hepatitis
Vectors
- Malaria
Specific Infectious Diseases after Disasters
- Measles
- Acute Respiratory Infection
- Cholera
- Shigellosis
- Malaria
- Typhoid
- Hepatitis
- Meningitis
In displaced populations 80 –90% of deaths occur due to 5 conditions:
- Malnutrition
- Measles
- Acute respiratory infection
- Diarrheal diseases (Cholera, Shigella)
- Malaria
Diagnosis and Treatment
As there are large numbers of patients, limited resources and austere conditions, one has to rely on
- Clinical Diagnosis
- Empirical Treatment
Measles –diagnosis
a. Fever
b. 3 Cs
- Cough
- Coryza
- Conjunctivitis
c. Rash
Measles Vaccination
Early in the emergency situation
– All children 6 months to 5 years
– Long term situations children 9 months to 5 years
– Any child vaccinated between 6 and 9 months -revaccinate at 9 month
If insufficient vaccine available, in order of priority
– undernourished children 6 month to 12 years
– all other children ages 6 to 23 months
– all other children 24-59 months
Concurrent vitamin A administration
Acute Respiratory Infections
Acute respiratory infections are a leading cause of death among effected populations. Pathogens involved are a variety of viruses and bacteria.
Control:
Provide adequate space, shelter, clothing, blankets, and ventilation
Cholera –Diagnosis
- Severe dehydration
- Rice water stools
- Painless
- Huge volumes
- Vomiting
Shigellosis –Diagnosis
- Bloody stools
- Cramps
- Fever
Malaria –Diagnosis
- Fever
- Jaundice
- Cerebral symptoms
- Renal failure
- Splenomegaly
Vector Control Methods
1. Habitat Control
2. Reducing Contact
3. Chemical Control
- Insecticides, larvicides, rodenticides
- Repellents
Insecticide use must be monitored by professionals
4. Biological Control
Physical screens can be used to control immediate problem. For the longer term -make environment less favorable for the vectors.
Following steps can be taken as well:
Improve personal hygiene through:
- Sanitation
- Drainage
- Garbage disposal
- Food storage and handling practices
- Remove stagnate water
- Camp location
Vector Borne Diseases
Disaster environments are very conducive to the proliferation of diseases-carrying insects and rodents (vectors).
Diseases such as malaria, filariasis, dengue, yellow fever, encephalitis, scabies, scrub typhus, plague, endemic typhus, relapsing fever, leptospirosis are vector borne.
Typhoid Fever –diagnosis
- Rose spots
- Fever
- Bradycardia
Hepatitis Diagnosis
- Fever
- Jaundice
- Malaise
Meningococcal Meningitis –Diagnosis
- Fever
- Headache
- Neck stiffness
- Purpuric rash
- Purulent CSF
 howMed Know Yourself
howMed Know Yourself