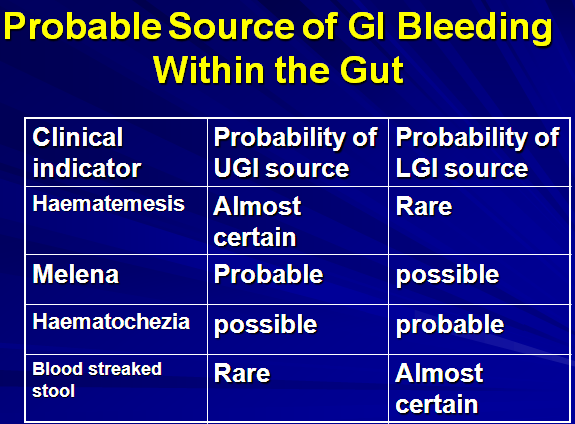
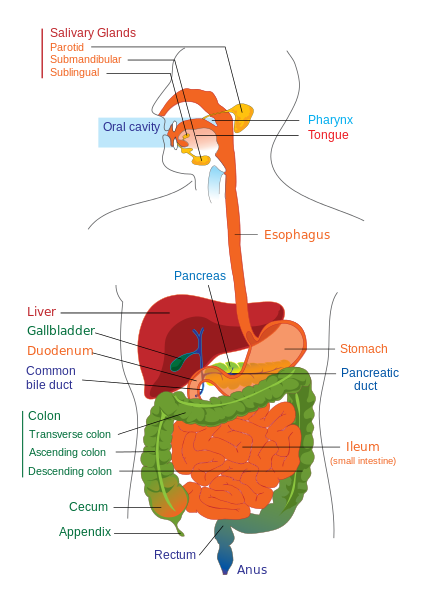
UGIB is bleeding derived from a source proximal to the Ligament of Treitz.
Photo by AJC1
Acute Upper G.I. Bleeding
- Haematemesis
- Melaena
- Haematochezia
Haematemesis
- The vomiting of blood.
- It indicates that the bleeding is from a cause proximal to the (LOT).
- The colour of the vomited blood is dependent on the concentration of HCL and its admixture with the blood .If the vomiting occurs soon after the UGIB , then haematemesis will be bright red in colour. IF there is a time lag then haematemesis will be dark red brown or black.
Melaena
- The passage of black and tarry stools.
- Usually due to UGIH.
- It results from more then 60-100 ml of blood with moderate transit time.
- Can be a result of LGIH if the GI transit time was sufficiently prolonged to about 8hrs.
Haematochezia
- The passage of fresh blood per rectum due to bleeding from the lower GIT.
- Rarely due to UGIB. Requires more than 1000ml.
GASTROINTESTINAL BLEEDING
- Hematemesis
- Melena
- Hematochezia
- Occult bleeding
Summary
- Vomiting of blood
- Bright red or dark
- Proximal to the ligament of Treitz
- Differentiate from hemoptysis, bleeding from mouth & pharynx
- 80-95% cases – Mucosal abnormalities, Varices, Spontaneous resolution
Causes of UGIH
- Esophageal Varices
- Duodenal ulcer
- Gastric ulcer
- Gastritis
- Other rare causes are:
- Mallory-Weiss tear.
- Boerhaave syndrome.
- Vascular Ectasia
- Aortoenteric fistula.
- Neoplasm
- Portal hypertensive gastropathy.
- Hemobilia.
CLINICAL PRESENTATION
- Clinical manifestations of GI bleeding depends upon extent & rate
- Postural hypotension suggests acute hemorrhage & intravascular volume depletion
- Fatigue & exertional dyspnea typical symptoms with slow, chronic blood loss
Symptoms and Signs
- Hematemesis – 40-50%
- Melena – 70-80%
- Hematochezia – 15-20%
- Syncope – 14.4%
- Presyncope – 43.2%
- Dyspepsia – 18%
- Epigastric pain – 41%
- Heartburn – 21%
- Diffuse abdominal pain – 10%
- Dysphagia – 5%
- Weight loss – 12%
- Jaundice – 5.2%
Clinical Features
History
Differentiate hematemesis from hemoptysis
Amount of blood loss (drops, tablespoonful, clots)
Recently ingested foods (food colors, beets, drugs)
Source of bleed (upper GIT, nose, mouth pharynx)
Prolonged, forceful vomiting (Mallory-Weiss)
Abdominal pain & vomiting (esophagitis, gastritis)
Cracked nipples, Jaundice & Liver disease
Umbilical vein catheterization (portal vein thrombosis)
Familial bleeding diathesis
PHYSICAL
- Orthostatic changes in pulse & BP
- Cardiopulmonary
- Skin
- Examine oral cavity & nasopharynx
- Lymph nodes
- Abdomen
- Digital rectal
Physical signs
- Petechiae, Ecchymosis
- Icterus, Palmar erythema, Spider angioma
- Hepatosplenomegaly, Ascites
- Active nasopharyngeal bleed
- Occult blood in stools
Approach to the patient
GOAL — Determine the cause & treat
Phase – 1 Differentiate (blood, food color, Beets etc)
Phase – 2 Assess severity (Hematocrit, Capillary refilling, Vital signs)
Phase – 3 Determine the site ( Epistaxis simulates Upper G I bleed)
Imaging, Endoscopy
Clinical Approach
- Confirm bleeding
- Assess Severity
- Resuscitate
- Medical Intervention
- Liaison with surgical/ ITC Team
- Diagnosis of site
- Surgical hand over
Hints for Screening
Make sure – vomited material: is it really blood ?
NG aspirate –ve for blood doesn’t rule out ‘UGIB’
Competent pylorus may mask a duodenal bleed
Bright red blood – active bleed
Dark ‘Coffee grounds’ – denatured by gastric acid
Rapid bleed – a medical emergency
Slower bleed – anemia, occult blood in stools, melena
Hypotension – may not be seen even in a large bleed
Initial Hb – values may be unreliable
Acute U.G.I. Bleeding
Clinical approach:
–1. if small amount, no immediate Tx, because CVS can compensate –
–2. 85% stop bleeding during 48 hrs –
–3. Criteria for low risk
- Age less then 60 years
- Coffee ground without malena
- Alcohol induced
- Hemodynamically normal
4. Criteria for Hospitalization
- –recent (24 hrs),
- –age (60 +)
- –Continuing visible blood loss.
- –Hemetemsis with malena
- –Cardio-respiratory disease
- –Signs of chronic liver disease
- –Shock
- P>100,BP<100
- Poor peripheral circulation
- JVP<1cm (from sternal angle when Patient is flat)
Immediate management:
** Emergency management:
History.
(Dyspeptic symptoms, Vomiting preceding blood, Alcohol, Drugs, Previous episode of bleeding, History of jaundice, peptic ulcer, surgery )
- Monitor: pulse & BP /30 min
- Blood sample: haemoglobin, urea electrolytes, grouping & cross-matching
- I.v. access
**Shock management:
- ABC
- Airway: endotracheal tube, oropharyngeal airway.
- *Give oxygen
- Breathing: support respiratory function
- * Monitor: resp. rate, blood gases, chest radiograph
- – Circulation: expand circulating volume: blood, colloids, crystalloids support CVS function: vasodilators
- * Monitor: skin color, peripheral temp., urine flow, BP, ECG
Blood transfusion in case of:
1) shock
2) haemoglobin <10 g/dl
- Urgent endoscopy
- Surgery when recommended
Rationale for Endoscopy
To identify the source of bleeding
To determine the risk of re-bleeding
To render endoscopic therapy
- Band ligation
- Injection sclerotherapy
- Cautery
- Heater probe
- Endoclip
General Investigations:
1. Hb, PCV
2. CBC (WBC … etc)
3. Bld glucose
4. Platelets, coagulation
5. Urea, creatinine, electrolytes
6. Liver biochem.
7. Acid-base state
8. Imaging: chest & abd. radiography, US, CT
Laboratory Aids
1. Bleeding scans – Inconclusive Endoscopy
Technitium sulfur colloid (detects rapid bleed)
Tagged RBCs (for small bleeds)
2. Angiography
General management:
–Drug therapy
1. H2 – receptor antagonists
2. proton pump inhibitors
3. octreotide
4. Vasopressin/Terlipressin
Factors in reassessment
1. age: 60 + indicates greater mortality
2. recurrent hemorrhage: +++ mortality
3. re-bleeding: mostly within the 1st 48 hrs
Further Evaluation
Re-bleeding Signs:
–Rise in pulse
–Decreased urinary output
–General condition deterioration
–Continued bleeding after 6-8 units of blood
–Spurting vessel at endoscopy
Treatment of Uncontrolled Bleeding
- Sengastaken– Blakemore tube
- TIPSS
- Surgical shunts
Prognosis
Overall mortality =8-12%
can be reduced to 6-9%
 howMed Know Yourself
howMed Know Yourself