Opportunistic mycoses are fungal infections that do not normally cause disease in healthy people, but do cause disease in people with weakened immune defenses (immunocompromised people). Weakened immune function may occur due to inherited immunodeficiency diseases, drugs that suppress the immune system (cancer chemotherapy, corticosteroids, drugs to prevent organ transplant rejection), radiation therapy, infections (e.g., HIV), cancer, diabetes, advanced age and malnutrition.
Species causing opportunistic infections include:
1. Candida
2. Cryptococcus
3. Aspergillus
4. Mucor & Rhizopus
5. Pneumocystis
Candida albicans
Candida albicans is the most important species belonging to Candida. C. albicans is a member of the indigenous microbial flora of humans. It is part of the normal flora of gastrointestinal tract, upper respiratory tract, buccal cavity and vagina, therefore no transmission is required. Growth is normally suppressed by other microorganisms found in these areas. Alterations of gastrointestinal flora by broad spectrum antibiotics or mucosal injury can lead to gastrointestinal tract invasion. Skin and mucus membranes are effective barriers but damage by introduction of catheters or intravascular devices can permit Candida to enter bloodstream. It causes localized as well as disseminated disease.
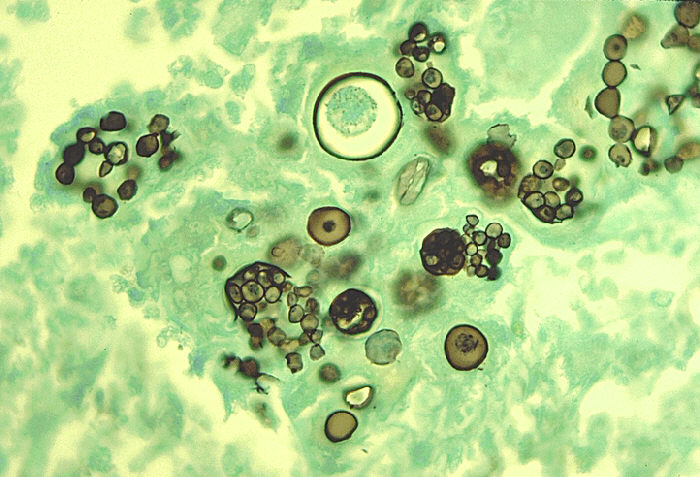
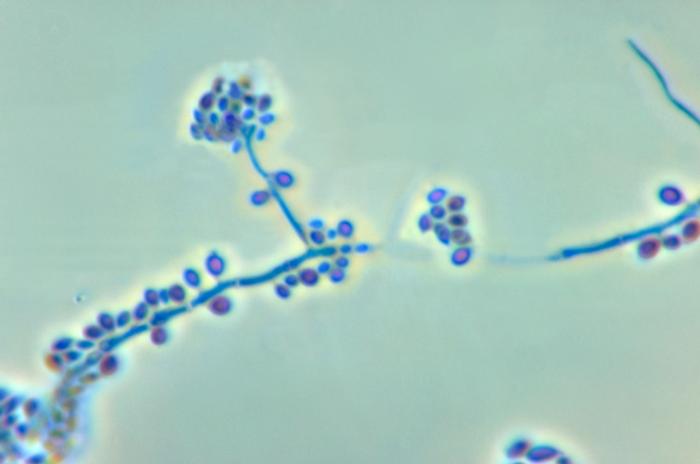
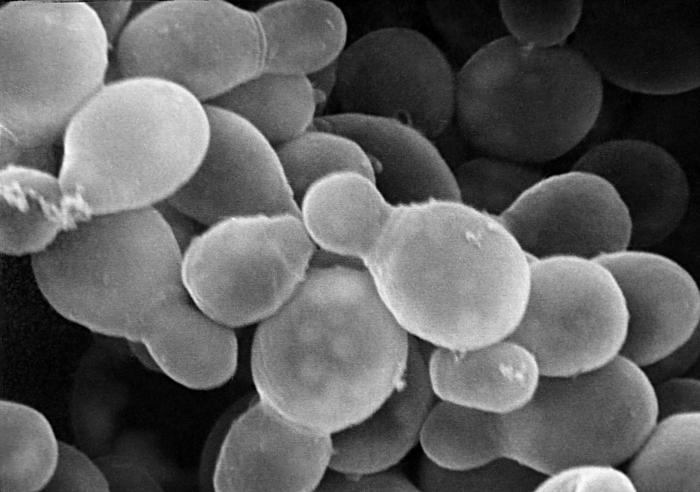
Candida albicans is an oval yeast with a single bud. In tissues, it forms pseudohyphae. Pseudohyphae are elongated yeasts and not true hyphae.
Thus it occurs in different forms at different temperatures:
- In vitro (25 C): mostly yeast;
- In vivo (37 C): yeast, hyphae and pseudohyphae
Risk factors for candidiasis
- Post-operative status
- Cytotoxic drugs
- Antibiotic therapy
- Burns
- Drug abuse
- Gastrointestinal damage
Infections
Localized infections include:
1. Thrush – oral candidiasis – a pseudomembrane
2. Vulvovaginitis (high pH, diabetes or overuse of antibiotics are risk factors)
3. Finger and nail infections
Candidia albicans may cause systemic or disseminated disease by dissemination to many organs. It may cause chronic mucocutaneous candidiasis or candida oesophagitis.
Chronic mucocutaneous candidiasis
Immunologic studies of patients with chronic mucocutaneous candidiasis often reveal defects related to cell-mediated immunity, but the defects themselves vary widely.
Chronic mucocutaneous candidiasis (CMC) is the label given to a group of overlapping syndromes that have in common a clinical pattern of persistent, severe, and diffuse cutaneous candidal infections. These infections affect the skin, nails and mucous membranes.

Laboratory Diagnosis
• Exudates may show yeast cells
• Tissues may include pseudohyphae
• On gram staining, these are gram positive
• Calcoflour white staining may be used as well
• On culture, form colonies resembling large colonies of Staphylococcus
• Germ tube test
Treatment
Treatment of choice is Fluconazole. Reduction of predisposing factors is also important.
Cryptococcus
Cryptococcus neoformans causes cryptococcal meningitis, the most common life threatening disease in AIDS patients.
C. neoformans is an oval budding yeast found in soil and pigeon droppings. There is no man to man transmission. It is surrounded by a wide polysaccharide capsule and is not dimorphic. It forms a narrow bud.
Organism is ubiquitous and infections occurs worldwide. C. neoformans is recovered in large amounts in pigeon droppings but does not cause disease in birds. The primary site of human infection is in the lungs. Although cryptococcal meningitis is most common disseminated manifestation, but can spread to skin, bone and prostate.
Cryptococcosis
Cryptococcosis is a chronic, subacute to acute pulmonary, systemic or meningitic disease, initiated by the inhalation of the fungus. Primary pulmonary infections have no diagnostic symptoms and are usually subclinical. On dissemination, the fungus usually shows a predilection for the central nervous system, however skin, bones and other visceral organs may also become involved.
It has worldwide distribution.
Laboratory Diagnosis
a. Direct Wet Preparation with use of India Ink
b. Gram stain is an unreliable method
c. Useful stains include methenamine silver, periodic acid-schiff (PAS) and mucicarmine.
d. On culture, forms highly mucoid colonies
e. Latex Agglunitaion Test
Treatment
Combined treatment with amphotericin B & flucytosine
Aspergillus
Genus occurs worldwide and contains hundreds of species. These species constitute the most commonly found fungi in any environment. Aspergillus fumigatus causes infections of the:
• Skin
• Eyes
• Ears
• Lungs -Aspergilloma or fungus ball, allergic bronchopulmonary aspergillosis (ABPA)
A. fumigatus exists only as molds and is not dimorphic. Septate hyphae are present and forms V shaped branches.
Major portal of entry is the respiratory tract. Dissemination can occur from the lungs and involve other areas of the lung, the brain, GI tract and kidney. CNS and nasal-orbital cavities can also become involved.
Aspergillosis
Aspergillosis is the most common fatal infection seen in patients with chronic granulomatous disease of childhood. Progressive and disseminated disease can complicate neoplastic diseases, especially acute leukemia, bone marrow and organ transplantation (not necessarily AIDS).
Aspergillosis is caused by Aspergillus fumigatus, A.flavus and other species.
Treatment
- Amphotericin B
- Caspofungin
- Surgical removal of fungal ball
Mucor & Rhizopus
Mucor and rhizopus cause mucormycosis including zygomycosis and phycomycosis. These are widely distributed moulds. Transmission is by airborne transmission.
Mucormycosis predisposing factor is diabetic ketoacidosis.
Treatment
- Treatment of the underlying disorder
- Amphotericin B
- Surgical removal of necrotic infected tissue
Pneumocystis
Many species are found in the genus pneumocystis. In humans, one named as P. jeroveci causes disease. In rodents, P. carinii is seen.
Pneumocystis a Fungus or a Protozoan??
- RNA and DNA studies are suggestive of a fungus but is medically thought to be a protozoan.
- It does not have ergosterol in its membranes as do fungi but has cholesterol.
- It forms cysts in tissues resembling protozoa.
- It does not grow on fungal media
- Antifungal drugs are ineffective
Transmission occurs by inhalation and infects lungs predominantly. Cysts induce an inflammatory response consisting primarily of plasma cells, hence also called plasma cell pneumonia.
It primarily affects patients with AIDS and premature or debilitated infants.
Clinical Features
- Sudden onset of fever
- Non productive cough
- Dyspnoea
- Tachypnoea
- Bilateral rales and rhonchi
- Chest X-Ray shows a diffuse interstitial pneumonia with “Ground Glass” infiltrates bilaterally.
Laboratory Diagnosis
- Stains poorly with gram stain
- Methenamine silver & giemsa stains are used to visualize cysts in tissue
- No serologic test is available
- Have not been grown in culture
Treated with Trimethoprim-sulphamethoxazole and prevented by aerosolized pentamidine.
Pneumocystis Pneumonia – Systemic Mycoses
Pneumocystis jiroveci is causative agent formerly referred to as P. carinii. These are obligate parasites. Majority of individuals exposed to P. jiroveci by age 5 develop pneumonia. Infection in immunocompetent is usually asymptomatic
These are common opportunistic fungal infection of AIDS patients. Presence of the disease is almost diagnostic for AIDS. Disease may result in death if left untreated.
Other Pathogenic Fungi
- Penicillium marneffei
- Fusarium spp
- Pseudallescheria boydii
- Scedosporium prolificans
 howMed Know Yourself
howMed Know Yourself