Subcutaneous mycoses are caused by accidental subcutaneous inoculation of causative fungi. Most of the causative agents reside in soil and vegetation. Granulomatous response occurs at the site of infection. The infection is usually confined to subcutaneous tissues, and only rarely causes systemic disease.
Major Forms of Subcutaneous Mycoses
- Sporotrichosis
- Chromoblastomycosus
- Mycetoma
- Phaeohypomycosis
Sporotrichosis
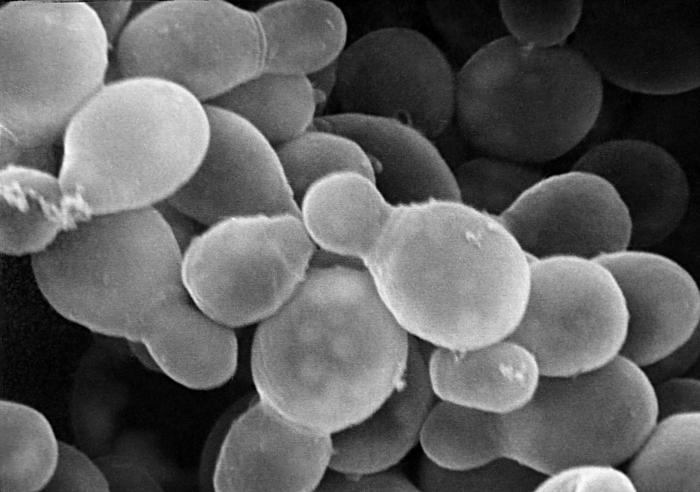
Sporotrichosis is caused by Sporothrix schenckii (a dimorphic fungus). This fungi is associated with plants, grasses, trees, sphagnum moss and rose bushes. At ambient temprature, it grows as a mold with branching septate hyphae and conidia. In tissues or in vitro at 35-37° C, it appears as a budding yeast.
Pathogenesis and Clinical Findings
The fungus is introduced in skin by trauma. Lesion is generally located on extremities (children often present with facial lesion). 75% lesions are lymphocutaneous and granulomatous nodule may progress to form necrotic lesions. Draining lymphatics become cord like with multiple subcutaneous nodules and abscesses along the course. Fixed sporotrichosis contain single nodule, and are less progressive, specially in endemic areas.
There is little systemic illness, rarely dissemination can occur in immunocompromised patients.
Diagnostic Laboratory Tests
Specimen include biopsy material or exudate from ulcerative lesion.
Microscopic Examination
- Direct microscopy with KOH or calcoflour white stain, yeasts are rarely found.
- Histopathological sections with Gomori methenamine silver or periodic acid schiff stain, yeasts are 3-5 µm spherical or elongated
Asteroid Body is seen in endemic areas with H&E stain, central basophilic yeast cell is surrounded by eosinophilic material.
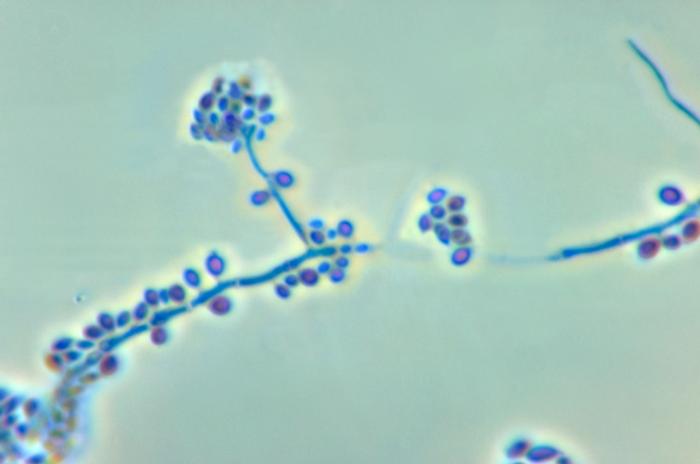
Culture
Culture is the most reliable method. Organism is inoculated on inhibitory mold agar or sabouraud’s agar with chloramphenicol, incubated at 25-30° C. Young colonies are blackish and shiny, becoming wrinkled and fuzzy with age. Branching septate hyphae with small conidia 3-5 µm are seen. Identification is confirmed by growth at 35°C and conversion to yeast form.
Serology
Agglutination of yeast cell suspension or latex particles coated with antigen with sera of infected patient (not always diagnostic)
Treatment
1. Usually self limited
2. Saturated solution of potassium iodide in milk
3. Oral Itraconazole or amphotericin B
Chromoblastomycosis
Chronic subcutaneous mycotic infection caused by traumatic inoculation of five Dematiaceous fungi having melaninized cell walls:
- Phialophora verrucosa
- Fonsecaea pedrosoi
- Rhinocladiella aquaspersa
- Fonsecaea compacta
- Cladophialophora carrionii
Lesion is granulomatous with hyperplasia of epidermal tissue
Pathogenesis and Clinical Findings
Organism is inoculated by trauma usually at legs or feet. Over months to years, lesion becomes wart-like and verrucous. Cauliflower-like nodules are formed. Crusting abscesses (black dots) of purulent material appear on surface. Rarely cause elephantiasis due to lymphatic obstruction.
Diagnosis
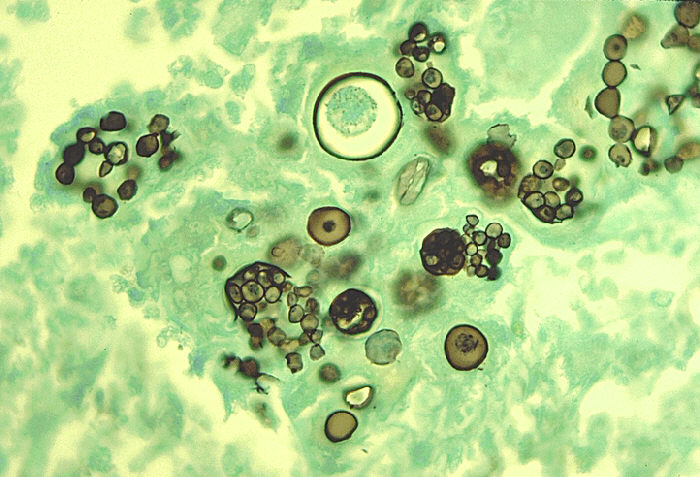
1. Specimen of scrapings or biopsies placed in 10% KOH and examined microscopically for dark spherical cells
2. Detection of sclerotic body (spherical brown cells) in tissue sections
3. Culture on SDA with chloramphenicol
4. Demataciaceous identified by characteristic conidial structure

Treatment
1. Surgical excision
2. Chemotherapy with Flucytosine and Itraconazole
Phaeohyphomycosis
Characterized by presence of dark pigmented septate hyphae in subcutaneous tissues.
Causative agents
- Exophiala jeanselmei
- Phialophora richardsiae
- Bipolaris spicifera
- Wangiella dermatitidis
Specimen are cultured on routine fungal media for identification.
Mycetoma
Mycetoma is the chronic fungal infection of skin, fascia, and bones of hands or feet. It is caused by mycelial fungi in the division Ascomycota. These fungi are found in the soil. Fungi introduced via traumatic inoculation from contaminated twigs, thorns, or leaves.
Clinical Features
- Nodules form at site of infection that slowly worsen and spread
- Draining sinuses containing granules
- Bone destruction can cause permanent deformity
Causative agents
- Pseudallescheria boydii
- Madurella mycetomatis
- Madurella grisea
- Exophiala jeanselmei
- Acromonium falciforme
Diagnosis
1. Microscopic examination of crushed granule
2. Culture on fungal media
Treatment
1. Surgical debridement
2. Chemotherapy
3. Antifungal Drugs
 howMed Know Yourself
howMed Know Yourself