Systemic mycoses are the systemic infections caused by fungi. Systemic fungal infections are caused mainly by:
- Histoplasma spp
- Coccidioides spp
- Blastomyces spp
- Paracoccidiodes
Many pathogenic fungi are dimorphic, forming moulds at ambient temperatures but yeasts at body temperature.
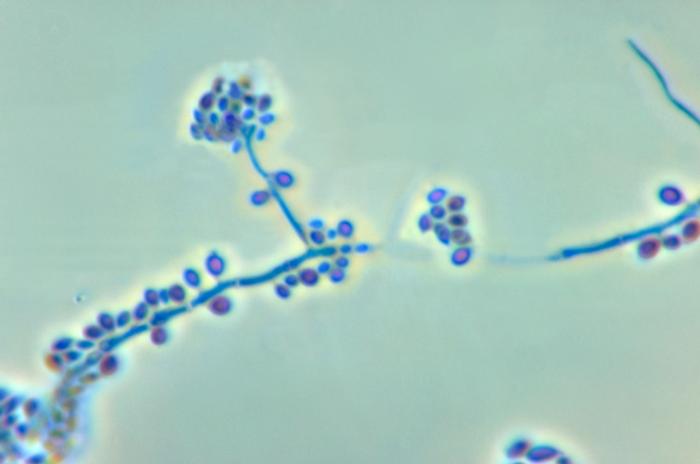
Coccidioidomycosis – Coccidioides imitis
Coccidioidomycosis is endemic in eemi-arid regions of Southwestern United States and similar climates in South and Central America.
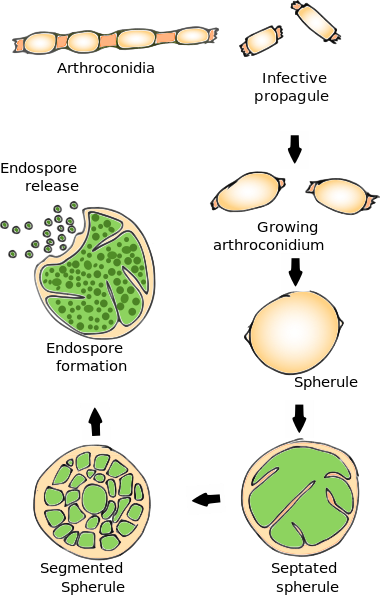
Pathogenesis
- Inhalation of arthroconidia (spores) present in soil
- 60% are asymptomatic, 40% as self-limited influenza- like illness called “San Joaquin Valley fever”
- Rash, erythema nodosum and erythema multiforme may appear
Coccidioidomycosis may be divided into the following types
- Primary pulmonary coccidioidomycosis – Acute allergic cutaneous lesions
- Disseminated coccidioidomycosis
- Primary cutaneous coccidioidomycosis
Disseminated Infection 0.5%
a) Skin
- verrucous granulomas
- erythematous plaques
- nodules
b) Musculoskeletal
Bone (40% disseminated)
- chronic presentation
- involve skull, metatarsals, spine, tibia
Joints
- involve monoarticular joints
- knee, wrist, ankle
- subcutaneous, muscle extension
Laboratory Diagnosis
a. Direct Examination of
- sputum
- tissue biopsy
- skin
- CSF
b. KOH staining
c. Calcofluor staining
d. Histopathology (GMS, PAS)
e. Culture at 30 C
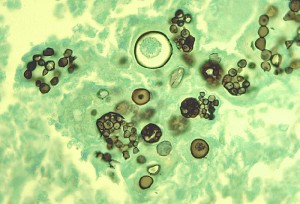
Histoplasma capsulatum
Histoplasma capsulatum, a dimorphic fungus, causes histoplasmosis, also called cave disease. Histoplasmosis is characterized by intracellular growth of the pathogen in macrophages and a granulomatous reaction in tissue. These granulomatous foci may become reactivate and cause dissemination of fungi to other tissues.
The distribution is world-wide, including United States, Mississippi Valley and St. Lawrence Valley. It is found in areas of heavy soil contamination by bird or bat excrement. Birds not infected, but bats may be symptomatic. Most infections are asymptomatic.
Histoplasmosis may be divided into the following types
- Primary pulmonary histoplasmosis
- Progressive disseminated histoplasmosis
- Primary cutaneous histoplasmosis
- African histoplasmosis
Diagnosis

1. Obtain appropriate specimens
- sputum
- blood
- urine
- biopsy specimens
- lesion scrapings
- bone marrow
2. Direct Examination of tissue specimens
◦ stains for fungi – PAS, GMS, Giemsa
◦ routine histology – H & E
Small yeast (2-4 microns) are found intracellularly in macrophages. Granulomas may be non-caseating or caseating.
For sputum, KOH or calcofluor staining is used.
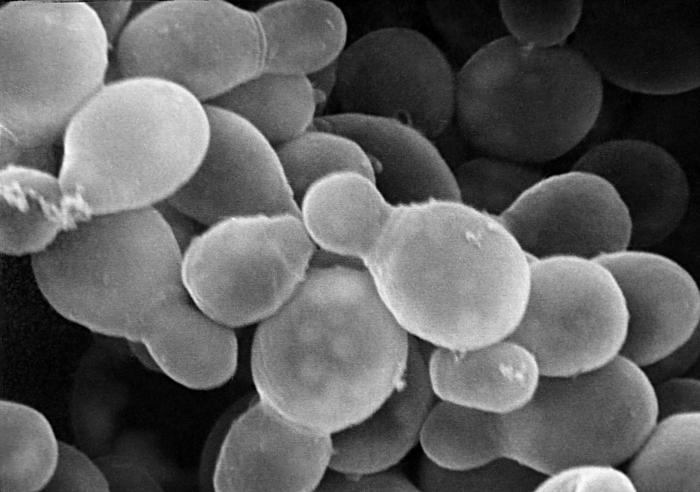
Blastomyces dermatitidis
Blastomycosis
Blastomycosis is a primary pulmonary infection. It may be mild and self limiting or disseminated disease with spread to bone, skin, lung and genito-urinary system. Chronic granulomatous lesion and suppurative infection is seen.
Inhalation of conidia is followed by conversion to yeast form, resulting in:
- Inflammatory response
- Non-caseating granulomas
- Pyo-granulomatous response
- Epithelioid & giant cells
Diagnosis
1. Direct examination -KOH and calcofluor tissue stains
2. Culture
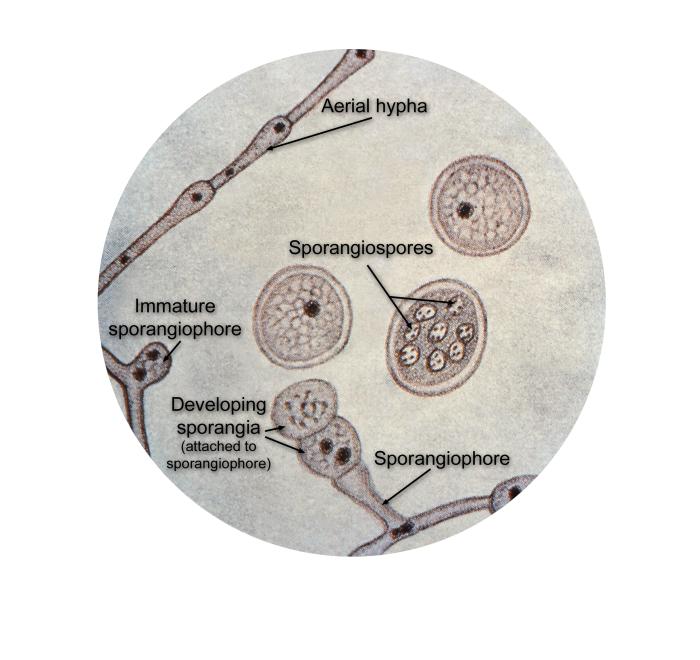
As undergo slow growth approximately 14 days up to 8 weeks are required. Mycelial form at 30 C is white to light brown. Conversion to yeast form at 37 C is necessary for identification. 1-2 µ conidia are also seen.
Immunodiffusion or molecular probe may also be used.
3. Serology
Serology is more likely to be positive later in disease (>6 wk).
- Complement Fixation Test (CFT)
- Immunodiffusion
- ELISA
Paracoccidioides immitis
Paracoccidioides brasiliensis is responsible for causing paracoccidioidomycosis. It is found in southern Mexico and regions of South America. Disease is found most in farm workers in endemic areas. It is similar to blastomycosis and coccidiodomycosis. The infection begins as a pulmonary condition. The fungus almost always spreads.
Pathogenesis
- Inhalation of conidia
- Initial lesions in lungs
- May remain dormant for decades
- Activation and progressive pulmonary disease and dissemination
- Involvement of skin, mucocutaneous tissue, lymph nodes, spleen, liver, adrenals, mouth
- Granuloma formation and microabscesses
 howMed Know Yourself
howMed Know Yourself