Antimicrobial Drugs
- Antimicrobial drugs are the greatest contribution of 20th century to therapeutics
- Advent has changed the out look of physicians about power of drugs over diseases.
- They are amongst the few curative drugs
- Importance is magnified in developing countries, as infectious diseases are present predominantly.
- These are the most frequently used/misused drugs
- Chemotherapy refers to the treatment of diseases by chemicals that kill the cells, specifically those of micro-organisms or cancer cells.
- If directed against cancer cells, we label it as cancer chemotherapy.
- If directed against micro-organisms, we call it antibiotics.
- Antibiotics are the natural substances produced by micro-organisms that kill or inhibit the growth of other micro-organisms. They are used in low concentration.
This definition excludes all substances produced by higher forms of organisms, like antibodies, and excludes those substances produced by micro-organisms but required in higher concentration to inhibit the growth of micro-organisms. E.g. ethanol, leptic acid, H2O2, etc.
Drugs in this class differ from all others since they are designed to specifically inhibit or suppress the infecting organism, without producing damage to recipient.
Drugs in this class differ from all others.
History of Chemotherapy
History has been divided into certain periods, these include:
Period of Empirical Use (1890-1935)
- Moldy curd was used by Chinese for treating boils.
- Chaulmoogra oil was used by Hindus for leprosy
- Chenopodium was used by Aztecs (Mexicans) for intestinal worms.
- Mercury was used by Paracelsus for syphilis, he is known as father of chemical chemotherapy.
- Cinchona Bark has been used since ancient times for treating fever.
- Antibiosis- Pasteur (1877)
The phenomenon of antibiosis was introduced by Pasteur in 1877. He showed growth of anthrax bacilli in urine was inhibited by air borne bacteria.
Ehrlich’s phase of Dyes and Organometallic compounds (1890 – 1935)
- This was the time when discovery of Microbes occurred. Ehrlich toyed with the idea that if certain dyes could selectively stain micro-organisms, then these will also be selectively toxic to micro-organisms
- He tried Methylene blue & Trypan red
- Developed Arsenicals; Atoxyl (for sleeping sickness), Arsphenamine & Neoarsphenamine (discovered 1906 and 1909 respectively for treatment of Syphilis)
- The term Chemotherapy was first used by Ehrlich since he used substances of known chemical structure and showed that selective attenuation of affecting parasite was practical.
Modern Era of Chemotherapy
- Ushered by scientist Domagk. He demonstrated therapeutic importance of Prontosil (sulfonamide) which was sulphonamide dye used in pyogenic infections.
- Soon it was realized that dye was a part and not essential in treating infection. Rather active moiety was para amino benzene sulfonamide
- First sulfonamide by name of Sulfapyradine – 1938.
- Fleming (1929) found that a diffusible substance was produced by a penicillium mold. This could selectively inhibit growth of staphylococci on culture plates. He named it Penicillin, but could not purify it
- Chain & Florey carried on the work and Clinical Use of Penicillin was started in 1941. Its commercial manufacture started in 1940s because of great potential in war wounds.
- Waksman & colleagues undertook research of Actinomycetes as source of antibiotics and aminoglycosides. Streptomycin comes into being in 1944 produced by Streptomycetes.
- This group of Soil-microbes proved to be a treasure house of many antibiotics and soon Chloramphenicol, tetracyclines and erythromycin were discovered.
- All three group of scientists Domagk, Fleming, Chain and Florey received Nobel prize
- In past 40 years emphasis has shifted from searching for new antibiotic producing organisms to semi-synthetic and synthetic derivatives of older antibiotics. They are said to have less adverse effects and more desirable properties.
- Synthetic antimicrobial agents like fluroquinolones and oxazolidinone have come up.
General Principles
Indication of chemotherapy
Prescriber should clearly identify whether there is need of chemotherapy or not, because some infections like sore throat, common cold have viral origin and hence there is no role of antibiotics. They themselves subside in 5-7 days if defense mechanisms are good enough. Symptomatic measures will help.
Selection of drug, dose & route of administration
Selection of drugs is based on cost effectiveness of drug, the safety and toxicity. We have targeted chemotherapy and empirical chemotherapy.
In targeted chemotherapy specific treatment is carried out based on culture sensitivity report. However facilities for culture sensitivity are not always available.
Empirical chemotherapy is based upon clinical practice, the experience of doctor, the epidemiological pattern of disease, extent of disease in community.
We take the specimen for culture but start treatment at the same time. Usually treatment is initiated with narrow spectrum drugs, however, in life threatening situations we start with broad spectrum antibiotics.
Selection of dose should be enough to achieve minimum inhibitory concentration (MIC). It is the
“Minimum concentration of antibiotic required to suppress growth of micro-organisms or to achieve therapeutic effect”.
Route of administration
Route of administration is such that MIC is achieved and the drug reaches the site of action. E.g. aminoglycosides like streptomycin if given orally, it is ineffective (a polar compound).
Drugs which cannot cross BBB can be given by intrathecal route of administration. However nowadays intrathecal administration can produce neurotoxicity so drugs like penicillin in meningitis are given I/V in massive doses. In this way desired concentration is achieved.
Duration of therapy
Most drugs are continued for more than 48 hours even after symptoms subside. In certain chronic diseases like tuberculosis, treatment is continued for 6-8 months and in leprosy treatment is given for one year.
Mono –drug therapy
Monotherapy is better tolerated. It is cost effective and chances of drug interactions are less.
Drug combinations
There are certain conditions where there is no concept of monotherapy, e.g. tuberculosis.
There are a few advantages of drug combinations:
- To achieve synergism
- There can be decreased toxicity if two drugs are combined. They have synergistic action, as lesser dose of individual drugs is required.
- It will prevent emergence of resistance to one drug
- To enhance antimicrobial spectrum.
Change of drug
Frequent change of drug is not a good practice. Enough time should be given to a drug so that it get absorbed, reaches the site of action and produces pharmacological effects.
Removal of barriers for site of administration
Sometimes barriers like presence of pus or necrotic tissue can decrease the effectiveness of antibiotics. E.g. drainage of pus makes treatment more effective.
Monitoring of plasma levels of drugs
This monitoring is of drugs where therapeutic index is low. Among antibiotics, it is frequently done with aminoglycosides and with certain cancer chemotherapy drugs.
Chemoprophylaxis
Prevention of diseases of infections by chemotherapy.
- Non-surgical
E.g. in patients of rheumatic fever long acting penicillin is drug of choice for preventing recurrences.
In meningococcal meningitis, ceftriaxone or Rifampicin is given during an epidemic. In malaria, person travelling to endemic area with high transmission rate, Mefloquine or Primaquine are given.
- Surgical-includes, purpose
Includes superficial incisional infections, deep incisional infections, organ or space infection
Purpose of surgical chemoprophylaxis is to decrease the incidence of surgical site infections, to decrease the adverse effects of drugs with minimum alteration of microbial flora.
Incidence of surgical infection is more where duration of surgery is 2 hours or more (prolonged surgery) or where there is insertion of prosthesis in bones or body cavities.
10. Treatment of carrier states
Carrier state is the continuous presence of micro-organisms like bacteria, viruses or fungi in organisms without infecting that person or producing symptoms, but capable of infecting or transmitting it to other persons.
E.g. meningococcal carrier states and typhoid fever carriers.
Classification
Classification can be according to:
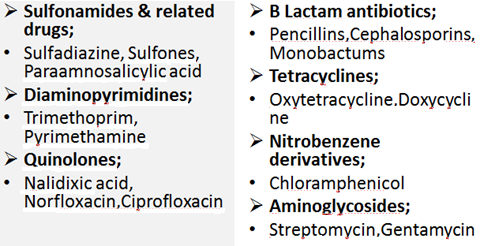
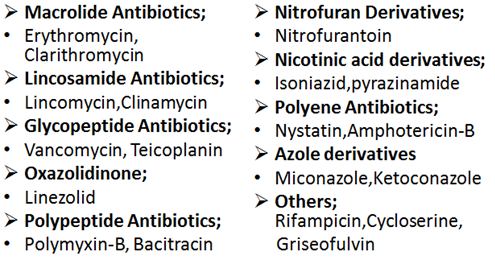
- Chemical structure
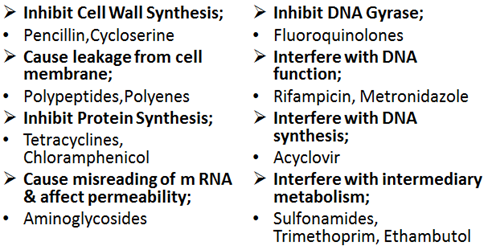
- Mechanism of Action
- Type of organism against which primarily active
- Spectrum of Activity
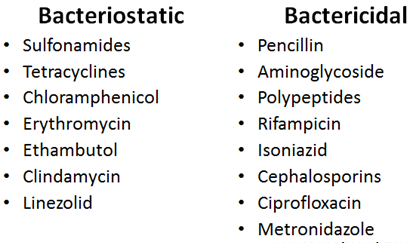
- Type of Action
- Source
Classification on basis of Chemical Structure
Classification on basis of Mechanism of Action
Type of organism against which primarily active
Antibacterial;
- Penicillin,
- Aminoglycosides,
- Erythromycin
Antifungal;
- Griseofulvin,
- Amphotericin B,
- Ketoconazole
Antiviral;
- Acyclovir,
- Amantadine
Antiprotozoal;
- Chloroquine,
- Metronidazole
Anthelminthic;
- Mebendazole,
- Niclosamide
Spectrum of Activity
- Narrow-Spectrum;
Drugs are effective only against certain specific families of bacteria. e.g. Streptomycin, Erythromycin
- Broad -Spectrum;
Drugs are effective against wide range of disease producing micro-organisms, against both gram positive and negative organisms. E.g. Tetracyclines, Chloramphenicol
Type of Action
Bactericidal drugs that kill bacteria.
Bacteriostatic drugs that only stop the growth of bacteria, not necessarily harming them otherwise.
Upon removal of bacteriostatic drugs, growth of bacteria is resumed.
Antibiotics are obtained from
Fungi;
- Penicillin form penicillium chrysogenum,
- Cephalosporin from Cephalosporium,
- Griseofulvin from another species of penicillium
Bacteria;
- Bacitracin from bacillus subtilis,
- Aztreonam from chromobacterium violaceum
Actinomycetes;
- Aminoglycosides,
- Macrolides,
- Tetracyclines,
- Chloramphenicol
Problems that arise with the use of Anti Microbial Agents
- Toxicity
Toxicity is divided into:
a. Local toxicity
Local irritation produced at site of administration e.g. pain and abscess formation by I/M drugs and thrombophlebitis of injected vein by I/V administration.
Almost all antimicrobials produce this toxicity. It is mostly seen with erythromycin, tetracyclines and cephalosporins.
b. Systemic toxicity
Almost all antimicrobials produce dose related and predictable organ toxicity. E.g. with aminoglycosides ototoxicity and nephrotoxicity is seen, with tetracyclines, renal and hepatic toxicity occurs and with chloramphenicol bone marrow suppression is encountered.
- Hypersensitivity reactions
Practically all antimicrobials are capable of producing hypersensitivity reactions, ranging from skin rashes to anaphylactic shock. These might be unpredictable and not related to dose. Usually seen with penicillin and cephalosporins.
- Super infection
Appearance of newer infection as a result of aminoglycosides since these drugs are capable of suppressing flora. It is seen with broad spectrum drugs. Individuals are compromised and situation is difficult to treat.
- Nutritional Deficiencies
With prolonged use of antimicrobial agents, vitamin B and vitamin K deficiency can occur. E.g. neomycin aminoglycoside can produce steatorrhoea and malabsorption syndrome.
- Masking of an infection
Aminoglycosides may be sufficient to treat one infection at same time mask another one acquired. One infection is treated at a time, as a result second infection manifests later in more severe form e.g. syphilis is masked by single dose of penicillin that is used to treat gonorrhea.
- Drug Resistance
Drug resistance is the unresponsiveness of micro-organisms to aminoglycosides. It is similar to the phenomenon of tolerance seen in higher organisms. It is basically divided into:
a. Natural Resistance
Some microbes have always been resistant to aminoglycosides due to lack of target site on which they act, due to alteration in metabolic processes. E.g.
- Gram –ve bacilli are not affected by penicillin.
- Mycobacterium tuberculosis is not affected by tetracyclines.
This type of resistance poses no significance clinically.
b. Acquired Resistance
Development of resistance due to use of aminoglycosides over a prolonged period of time. This is dependent upon the micro-organisms.
Some bacteria are notorious for rapid acquisition of resistance like Staphylococcus aureus, coliforms and tubercle bacilli.
However, some like Streptococcus pyogenes and Spirochetes have not developed resistance to penicillin though they have been exposed to it for more than 50 years. Thus have slow acquisition of resistance
- Gonococci quickly develop resistance to suphonamides. They slowly develop resistance to penicillin.
Genetic alterations leading to drug resistance
Drug resistance may be due to mutations and genes transfer.
1. Mutations
Stable, heritable genetic change that occurs spontaneously and randomly among micro-organisms and are not induced by antimicrobial agents. Any sensitive population of micro-organisms contain a few mutant cells which require a higher concentration of antimicrobial agents for inhibition. These cells are selectively preserved and get a chance to proliferate once sensitive cells are removed. This mutation may be single step or multiple steps.
a. Single step
It emerges rapidly, confers a high degree of resistance e.g. the resistance to Rifampicin develops in a single step manner.
b. Multistep
In this a number of gene modifications are involved. Sensitivity decreases in a stepwise manner. Resistance to erythromycin is developed by this manner.
2. Gene transfer
In gene transfer, infection may be transferred from one organism to another by:
a. Conjugation
Largely occurs in colon where a large number of gram negative bacilli come into contact. It is a very important mechanism of horizontal transfer of infection.
b. Transduction
Resistance properties are usually encoded in extra chromosomal “resistance factor”. Resistance factor is taken up by a phage and transferred to another bacteria. This transfer of resistance carrying gene through an agency of bacteriophage is called transduction.
c. Transformation
Infectious bacteria release the gene carrying resistance into a medium from where this is imbibed by another organism.
3. Altered expression of proteins in drug-resistant organisms
a. Modification of target sites
E.g. the alteration in penicillin binding proteins (PBP) in methicillin resistant staphylococcus aureus.
b. Decreased accumulation
Decreased accumulation of antimicrobial agents due to decreased entry or due to efflux pumps. E.g. in gram negative bacilli there is lipopolysaccharide layer that prevents the entry of aminoglycosides.
Presence of efflux pumps which pump the drug out of cells. It is seen with tetracyclines and primaquine.
c. Enzymatic Inactivation
Certain enzymes produced by microorganisms tend to inactivate aminoglycosides. E.g. beta lactamases inactivate penicillin and cephalosporins. Acetyl transferrase converts chloramphenicol into inactive compound.
4. Cross resistance
This is development of tolerance or resistance to toxic substances as a result of exposure to similarly acting substances. It is usually seen with pesticides and antimicrobial agents. E.g. Rifampicin and Refabuten cross react in treatment of tuberculosis. This cross resistance is because they are chemically and mechanistically related.
This cross resistance may be:
- Complete
E.g. resistance to one sulfonamide means resistance to all sulphonamides. Resistance to one tetracycline means resistance to all other tetracyclines.
- Partial
Partial cross resistance is usually seen when drugs are unrelated. E.g. seen between chloramphenicol and tetracylines.
Prevention of drug Resistance
- No inadequately prolonged use of antimicrobial agents.
- Prefer rapidly acting & selective aminoglycosides whenever possible.
- Use combinations especially when prolonged therapy is to be undertaken
- Organisms notorious for resistance like staphylococcus aureus and E. coli should be treated intensively.
 howMed Know Yourself
howMed Know Yourself