Diabetes Mellitus
Derived from Greek word diabainain: to pass through
It is a state of high glucose levels which may lead to complications including:
- Atherosclerosis
- Renal failure
- Changes in eye
- Retinopathy
- Ischemic heart disease
- Ultimately coma and death
Patient shows an increase in blood glucose levels due to decreased utilization of glucose, leading to increase in compensatory mechanisms, resulting in increased fat metabolism, leading to formation of ketone bodies (Acetone, Acetoacetic acid, alpha ketobutyric acid). This leads to ketoacidosis and death of patient.
Symptoms of Diabetes Mellitus
Main symptoms occur when absolute or relative deficiency is seen due to various factors:
- polyuria
- polydipsia
- glycosuria
Treatment
To give insulin. Increase in glucose levels occur due to relative deficiency of insulin. The purpose is to increase glucose metabolism and decrease fat metabolism.
Types of Diabetes Mellitus
Two types:
- Type-I (IDDM)
Absolute deficiency of insulin due to degeneration of pancreas, usually occurring in young age. It may be due to:
- Viral infections
- Autoimmunity
Insulin is required for treatment, so known as IDDM.
- Type-II (NIDDM)
Occurs in middle age, relative deficiency of insulin occurs. Although production may be normal but insulin antagonists may be present in blood. It is a less severe disease than type 1. Type II may lead to ketoacidosis. Insulin may not be required for treatment, it is usually due to increased activity of pancreas (overactiivty). Also has genetic basis.
Causes of insulin lack:
1. Lack of secretion –degradation of beta cells of pancreas
2. Tissues insensitivity to insulin mainly due to excessive secretion from pancreas (esp. type II occurring due to overeating)
3. Excess of insulin antagonists
a. Glucocorticoids
b. catecholamines
c. GH
d. oral contraceptives
4. Depressed release of insulin and transport
Increased blood glucose levels especially after meal is the main stimulus for the release of insulin.
It is mainly synthesized in beta cells of pancreas from pro-insulin, which comes from pre-proinsulin.
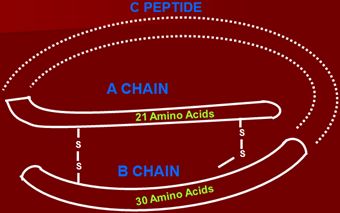
Insulin structure
It has a molecular weight of 5808. Chemically consists of 2 polypeptide chains:
- a chains –consisting of 21 amino acids
- b chains –consisting of 30 amino acids
linked together by disulfide bonds.
Mechanism of action
When insulin is released by beta cells on pancreas, it goes to target tissues present mainly in:
- liver,
- fat (adipose tissue)
- muscles
These contain insulin receptors. Concentration of receptors varies with the amount of insulin in blood. It is inversely proportional to the levels of insulin in blood.
If insulin is increased, downregulation of receptors occurs, leading to decrease in receptors.
After insulin release, it binds insulin receptors present on cell membrane of tissues. There are 2 parts of these receptors:
- alpha part –outside cell membrane
- beta part –transmembrane
Insulin binds alpha part. Due to binding, autophosporylation of beta part takes place.
Beta part is a kinase enzyme. When autophosphorylated, it also causes phosphorylation of other cell constituents in cell membrane, ultimately leading to translocation of glucose transporters from storage sites to cell membrane.
When these glucose transporters are transported, they cause increased utilization of glucose.
Pharmacokinetics
Polypeptide hormone, thus it cannot be given orally.
Routes Of Administration Of Insulin
- S/C, I/V, I/M but mostly given subcutaneously. In emergency I/V given.
- Implantable pumps
- Insulin pens containing catridges filled with insulin
- Insulin snuffs (inhalation –newer mode)(onset 30 min, peak 2-2.5 hr, duration 6 – 8 hr)
- Miniaturised infusion pumps
- Half life of 5-10 minutes
- Metabolized by insulinase enzyme in liver and kidney.
- Most of insulin secreted by pancreas enters portal veins and goes to liver, only 15% reaches systemic circulation.
- When given subcutaneously, entry into liver and other organs is same, thus this route is preferred.
- Addition of certain metals to prolong duration of action e.g. zinc is added to increase duration.
- Protamine zinc insulin is a type of long acting insulin.
Insulins Types: (According To Source)
- Bovine
- Porcine
- Human (recombinant DNA)
a) Bovine differs from human insulin in 3 amino acids.
b) Porcine differs from human insulin in 1 amino acid
c) Human insulin is pure form –formed by recombinant DNA technique
Disadvantage of bovine and porcine form is although having same effect but increased chances of hypersensitivity reactions.
Human insulin
- Has rapid onset of action
- Has short duration of action
- Is less immunogenic –no or less hypersensitivity reactions
But human insulin is very expensive, so as there is no difference in action, we always use bovine and porcine forms, being cost effective. Human form is resorted to only when patient is not responding or when hypersensitivity reactions are seen.
Bovine and porcine in pure form are mono component, causing less hypersensitivity reactions as compared to older preparations. Human insulin is in pure form, so has no reactions.
Classification (According To Duration Of Action)
- Ultra short acting
- Short acting
- Intermediate acting
- Long acting
| Preparation | Onset of Action | Peak Effect | Duration of action | ||
| Ultra – short acting | |||||
| Insulin lispro
Insulin aspart Glulisine |
20min | ½ hour | 3-4 hrs | ||
| Short acting | |||||
| Soluble insulin | ½ – 1 hour | 4-6 hrs | 8-10 hrs | ||
| Insulin zn suspension
Semilente |
|||||
| Intermediate acting | |||||
| NPH (isophane) | |||||
| Insulin zn suspension lente | 2hrs | 6-10 hrs | 24 hrs | ||
| Long acting | |||||
| Protamine zn insulin (pzi) | 4 hrs | 10-8 hrs | 36 hrs | ||
| Insulin zn suspension
Ultralente |
|||||
| Glargine | 2-5 hrs | 5-24 hrs | 18-24 hrs | ||
| Insulin mixtures | |||||
| Humulin 70/30 mix (30% soluble Insulin with 70% isophane)
Mixtard 30 HM (30% soluble Insulin with 70% isophane) |
Variable actions Depending on Predetermined Proportions of Short/intermediate or Intermediate/long acting Insulin | ||||
Doses Of Insulin
Preparations of insulin are available in the form of units. One unit of insulin is defined as:
“amount of insulin required to lower blood glucose level of a 2 kg normal rabbit from 120 – 45 mg/dl”
- Normal amount secreted by pancreas daily is 30 -50 units/d (0.5 -0.8 units/kg) of soluble (regular) insulin
- In IDDM, dose normally ranges between 30-50 units of insulin daily, depending on:
- Levels of blood glucose
- Physical activity of patient
- Diet of patient
When blood levels are more than 300mg/dl, start with 20 units of regular short acting insulin.
If blood levels are less than 200-300/dl, start with 10 units of regular insulin, with 4 units daily increments until blood levels are controlled.
- Long acting insulins given 10-14 units/day: dose increment 4 units on alternate days
- Ideally a combination of regular and long acting insulins is used twice daily. (regular –rapid onset, long acting –sufficient for delayed action)
- Once dose is adjusted, two-third dose is given in morning before breakfast and one-third before evening meal.
Adverse effects of insulin
- Hypoglycemia
When there is change in requirement of insulin, e.g.
- patient misses a meal,
- increased physical activity
he may go into hypoglycemia. Due to release of catecholamines, certain symptoms appear:
- tachycardia
- sweating
- anxiety
- apprehension
- insomnia
- headache
- in severe cases coma ‘hypoglycemic coma’ or even death may occur
Treatment
- give (if conscious) sugar, glucose or meal
- if unconscious, glucose given I/V, usually 30% glucose given by I/V drip or infusion
- most important is to educate the patient, as there may be damage to brain:
- not to miss meals
- always keep sugar, glucose to avoid
- no increase in physical activity or excessive physical activity
- whenever feels sympotms, take sugar to avoid hypoglycemia
- Lipodystrophy
Repeated injection at same site. Advised not to take injection at same site.
- Allergy
Animal origin –skin rash, articaria, localized or generalized
- Obesity (increased appetite)
May cause weight gain of patient
Treatment Of Diabetic Ketoacidosis
When treatment is not given, breakdown of fats cause diabetic ketoacidosis, which may be serious enough to cause death of patient.
1. Soluble/short acting Insulin:
Severe Ketoacidosis: 0.1 unit/kg/hr or 7 unit/hr
Less severe: 3 unit/hr
I/V drip: 40 units/l
Rapidly acting in medical emergency.
2. I/V fluids and electrolytes: Isotonic saline
5 L total fluid deficit: 500 ml Ist 20 min
2 L 90 min
1 L 90 min
1 L 120 min
3. Potassium: KCl I/V infusion 15mmol/hr by slow infusion, carefully monitored, given in hypokalemia.
4. Bicarbonate: If plasma PH< 7.0
Forms of human insulin (depending on source recombinant DNA technique)
- emp (enzyme modified porcine)
- prb (proinsulin recombinant in bacteria)
- pyr (precursor insulin yeast recombinant)
Mostly used for type II diabetes –all are taken 30 minutes before meal.
 howMed Know Yourself
howMed Know Yourself