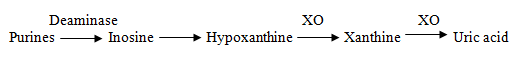
Gout is a disease of purine metabolism, necessary for DNA and RNA synthesis, characterized by:
- Hyperuricemia
- Recurrent attacks of acute arthritis
- Deposition of monosodium urate crystals in subcutaneous tissues, known as tophi
If remains untreated, there are chances of joint deformity.
Difference between rheumatoid arthritis and gout
| Rheumatoid arthritis | Gout |
| Incidence is more common in females | more common in males |
| Post menopausal | 30 years peak age |
Signs and symptoms
- Involvement of singe joint, usually 1st metacarpopharyngeal joint, big toe
- Pedegra (excruciating pain, swelling)
- Red and tender in acute phase, it becomes difficult to differentiate gout and cellulitis.
- Definitive when monosodium urate crystals from aspiration for gout.
- Subsides after some time, person becomes normal, then comes again.
On average, 5g purines are synthesized by body, 0.5 g are excreted and 4.5 g are recycled.
One enzyme is HGPRT (hypoxanthine guanine phosphoribosyl transferrase). In some deficiency of this enzyme leads to syndrome known as Lesch Nyhan syndrome. There are neurological problems as well.
People having primary gout have either relative or absolute deficiency or over activity of enzymes.
People with secondary gout also have some hereditary component.
Famous sufferers include Isaac Newton, Martin Luthar, Benjamin Franklin (introduced colchicine)
Drug Treatment of Gout
Causes of Hyperuricemia
Hyperuricemia is associated with gout, but every sufferer of hyperuricemia does not have gout.
Secondary causes
- Decreased renal excretion
- Drugs like diuretics are actively secreted at proximal tubule (thiazide, furosemide) 80% uric acid is actively secreted and most is reabsorbed.
- Low dose aspirin
- Pyrazinamide
- Cyclosporine
- Niacin
Lactic acidosis
- Alcohol
- Exercise
- Vomiting
- Starvation
Increased production of uric acid
Myeloproliferative disorders e.g. polycythemia
Lymphoproliferative disorders like CLL, psoriasis
Pathogenesis
Hyperuricemia causes increase in monosodium urate crystals, which are phagocytosed by synovial sites, producing prostaglandins and interleukins (inflammation). Chemotaxis of polymorphs makes the environment more acidic, which further enhances the precipitation. Further mediators of inflammation are released causing:
- Activation of chemotactic factors
- Production of lactic acid
- Release of lysosomal enzymes
- Glycoprotein synthesis
Treatment
Acute Gout
Specific
Colchicine
Non-specific
Indomethacin
Phenyl butazone
Ibuprofen
Piroxicam
Corticosteroids
Triamsinolone –orally, if not infective intra-articular injection
- Aspirin in low doses inhibits uric acid excretion.
- In higher doses decreases reabsorption -uricosuric effect
Both are undesirable.
Paracetamol is not used
Tolmetin is not used
Oxprozen is not used
Drugs used for Chronic Gout
Allopurinol
Febuxostat –newer drug
Uricosuric agents
Probenecid
Sulphin pyrazone
Benzbromarone
IL-1 inhibitor
Anakinra
Colchicine
Specifically meant for acute attack of gout. It is not analgesic and relieves pain by controlling inflammation.
- Very narrow therapeutic index so fallen out of favor
- Hardly available
Source alkaloid obtained from Colchicum autumnale
Mechanism of Action
In acute inflammation for migration and macrophage functions.
Microtubules are required, polymerization of tubulin occurs. When colchicine binds tubulin, it prevents polymerization. Both chemotactic and phagocytic functions of macrophages are lost, thus
- Controls inflammation and
- Rapid proliferation of these inflammatory cells
For cell division, microtubules are required, as are inhibited, thus cell proliferation does not take place.
- Also inhibit leukotrines B4 by unknown mechanism.
Thus used for treatment of acute gout.
Pharmacokinetics
Well absorbed orally. Also used I/V.
Dose 0.6 mg initially. 0.6 mg after every two hours, till acute attack subsides. As little as 8 mg can be fatal.
Metabolites are partly excreted through liver, and partly through kidneys.
Side effects
- GIT intolerance –where cells are rapidly dividing, nausea, vomiting, diarrhea, abdominal pain -1st sign of acute toxicity.
- Bone marrow suppression
- Hair loss
- Peripheral neuritis
Acute toxicity
- Burning throat pain
- Hypotension
- Shock
- Oliguria leading to hematuria
- Ascending CNS paralysis occurs because of respiratory paralysis
Treatment
Only supportive
Probenecid and Sulfinpyrazone
Weak acids having similar mechanism of action.
Mechanism of action
Uric acid is freely filtered partly at glomerular membrane. 80% is actively secreted and reabsorbed at PCT. These drugs block the reabsorption of uric acid. More uric acid is lost in urine. So known as uricosuric agents. They are very useful in individuals who are underexcretors of uric acid. If less than 800 mg/24 hours uric acid is excreted in urine, then known as underexcretors.
For determination, have to take 24 hour urinary sample.
Adverse effects
- GIT irritation
- Allergic dermatitis
- Uric acid stones –as greater uric acid may precipitate. Before starting treatment it is checked whether person does not have problem already. There are two remedies to counter this side effect:
- Increased urinary volume (increased water intake)
- pH of urine is kept above 6.
- Aplastic anemia
Allopurinol
Inhibits uric acid production. Itself is acted upon by xanthine oxidase, converted into alloxanthine, which is active metabolite with a half life of 18-30 hours. Drug is needed to be given once a day. Alloxanthine inhibits xanthine oxidase
Once inhibited, relative increase in hypoxanthine and xanthine occurs, which are soluble and easily excreted through kidneys.
Indications
Chronic tophaceous gout
Severe disease characterized by monosodium urate crystals and tophi. If uric acid production is decreased, tophi resolve. As urate pool goes down, it enters plasma, thus in high uric acid excretors (more than 800mg/day) allopurinol is very effective.
In those individuals in whom uricosuric agents are contraindicated or have recurrent renal stones or impaired renal functions, sulphinpyrazzoles cannot be used.
There is gross elevation of uric acid levels.
Dose
100 mg/day, may be increased to 300 mg/once a day.
Side effects
1. Precipitation of acute gout
Fluctuating levels in plasma are more dangerous than simple hyperuricemia. Phagocytosis by synovial sites is increased. Allopurinol use decreases plasma uric acid levels, fluctuation in levels occurs, resulting in chances of precipitation of acute gout.
Whenever allopurinol is given in chronic case, initially it is combined with Indomethacin or Colchicine, to guard against this.
2. GI intolerance
a. nausea
b. vomiting
c. diarrhea
3. Allergic reactions
4. Bone marrow suppression
5. hepatic/renal toxicity
Drug interactions
Especially with anticancer drugs. In all types of cancers, there is increase in uric acid as well as increase in cell turnover, thus allopurinol has to be used. Mercaptopurine and Azathioprine are themselves metabolized by xanthine oxidase. Dose has to be reduced.
The dose of cyclophosphamide has to be reduced when allopurinol is given along with it.
Febuxostat
Non-purine inhibitor of xanthine oxidase. Similar mechanism of action to allopurinol, but is more selective and lower dose is required.
Dose 80-120 mg/day.
Adverse effects
- Nausea
- Diarrhea
- Impaired liver functions (transient rise in ALT, AST)
- Headache
Anakinra
It is under investigation and is interleukin 1 inhibitor. Interleukin 1 is released at start of gout, it is thought that it might be fruitful to use it in gout.
 howMed Know Yourself
howMed Know Yourself