What Are Hormones?
- Chemicals that are released into the bloodstream
- Regulators of specific body functions
Thyroid
Thyroid is the largest endocrine gland in human body, situated in front of neck. Isthmus divides it into two parts. It is mandatory for body temperature, regulation, metabolism, growth, reproductive system, etc.
In absence of thyroid, hypothyroidism occurs. If hormones are deficient at birth, congenital abnormality occurs. Cretinism appears in children. Thyroid hormones, if deficient, are replaced at birth to avoid mental and growth retardation.
Hormones
Secretes three hormones:
- Calcitonin, important in calcium homeostasis.
- Triiodothyronine (T3) and thyroxine (T4), important in growth and metabolic function.
It is composed of large number of follicles filled with coli. Major constituent glycoprotein is thyroglobulin, secreted by the cells into coli.
Iodine:
- Sources: Iodized table salt, dairy products, fish
- Adult requirement: 150 mg, increased to 200 mg in pregnancy.
- Iodized salt: 1 part sodium iodide added to 100,000 parts NaCl.
- The average dietary intake – 500 mg /day
- Dietary intake below 10 mg /day -synthesis of thyroid hormones inadequate
- After ingestion, readily absorbed from small intestine
- From extracellular pool, rapidly enters thyroid gland (trapping). After trapping, 30 times more iodine is present in gland than plasma.
- Enters through basement membrane (NaI symporter), an apical membrane another symporter pendrin is present, which controls outflow of iodide from cell.
- Transporter is also present in cochlea of inner ear à congenital absence leads to deafness and goiter.
- Different enzymes are involved in three steps:
- Oxidation in cells by peroxidase enzyme
- Organification –binding of iodide with tyrosine in thyroid leading to formation of monoiodotyrosine and diiodotyrosine.
- Coupling of MIT and DIT to form T4 and T3, which are stored in gland. When required, released in blood by proteolysis.
- In periphery deiodination occurs (T4àT3), reused.
Thyroid Hormones
- Cell membranes receptors: increase amino acid and glucose uptake.
- Inner mitochondrial membrane receptors: regulate energy metabolism.
TSH
- T4 & T3 are feed-back regulators of TSH
- TSH is stimulated by α-adrenergic agonists
- TSH secretion is inhibited by:
- Dopamine
- Bromocriptine
- Somatostatin
- Corticosteroids
Conversion of T4 to T3 is decreased by:
- Acute & chronic illnesses
- β-adrenergic receptor blockers
- Starvation & severe protein energy malnutrition (PEM)
- Corticosteroids
- Propylthiouracil
- High iodine intake (Wolff-Chaikoff effect)
Thyroxine (T4)
Total T4 level is decreased in:
- Premature infants
- Hypopituitarism
- Nephrotic syndrome
- Liver cirrhosis
- PEM
- Protein losing entropathy
Total T4 is decreased when the following drugs are used:
- Steroids
- Phenytoin
- Salicylates
- Sulfonamides
- Testosterone
- Maternal TBI (thyroid binding immunoglobulins)
Total T4 is increased with:
- Acute thyroiditis
- Acute hepatitis
- Estrogen therapy
- Clofibrate
- Iodides
- Pregnancy
- Maternal TSI
Goitrogens
Food
- Soybeans
- Millet
- Turnip,Mustard
- Cabbage
Thyroid Hormones
- 99% of T3 and T4 are bound to plasma proteins (thyroid-binding globulin).
- 0.04% T4 and 0.4% T3 occur in free form.
- They are excreted in the bile and urine.
- T4 has a half-life of 6-7 days; T3 has a half-life of 1-2 days.
- Oral absorption of T4 is 80% and T3 95%
- Readily absorbed from GIT and excreted in bile and urine.
- Some of the circulating T4 is deiodinated to T3, the more potent and rapidly acting form.
- 5:1 is the ratio of T4:T3 in thyroid.
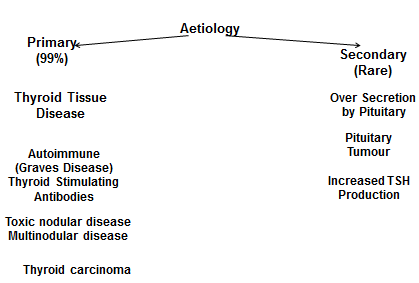
Hyperthyroidism
Excess of thyroid hormones or over-production.
Common Signs and Symptoms of Hyperthyroidism
- Nervousness
- Irritability
- Difficulty Sleeping
- Bulging Eyes
- Unblinking Stare
- Goiter
- Rapid Heartbeat
- Increased Sweating
- Heat Intolerance
- Unexplained Weight Loss
- Scant Menstrual Periods
- Frequent Bowel Movements
- Warm, Moist Palms
- Fine Tremor of Fingers, clubbing
Emotional Symptoms of Hyperthyroidism
- Nervousness
- Restlessness
- Anxiety
- Irritability
- Sleeplessness or insomnia
- Exhaustion
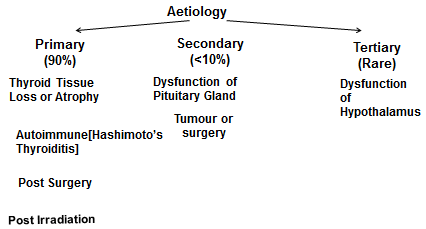
Hypothyroidism
It is reversible in adults. Slowing down of all body functions occurs. It is irreversible in children, as creatinism may occur.
Detected by:
- Low free thyroxine levels
- Elevated TSH
Common Signs and Symptoms of Hypothyroidism
- Tiredness
- Loss of Interest and/or Pleasure
- Forgetfulness
- Dry, Coarse Hair
- Loss of Lateral Eyebrow Hair
- Puffy Face and Eyes
- Goiter
- Slow Heartbeat
- Dry Skin
- Cold Intolerance
- Weight Gain
- Heavy Menstrual Periods
- Constipation
- Brittle Nails
How to Remember Signs and Symptoms of Hypothyroidism
Sleepiness, Fatigue, Lethargy
Loss of Memory, Trouble Concentrating
Unusually Dry, Coarse Skin
Goiter (Enlarged Thyroid)
Gradual Personality Change, Depression
Increase in Weight, Bloating or Puffiness (Edema)
Sensitivity to Cold
Hair Loss, Sparseness of Hair
Thyroid Drugs
- Replacement therapy.
- Treatment for hypothyroidism.
- Suppress TSH secretion.
- Levo isomers are more potent in increasing basal metabolic rate.
Once absorbed, their pharmacokinetic and dynamic properties are identical to endogenous thyroid hormones.
Shelf life is 2 years.
Levothyroxine
- Synthetic levo isomer of T4.
- Oral and I/V preparations are available.
- Low cost & content uniformity.
- Better standardization & stability and long duration.
- Long half-life of T4(7 days)
- Facilitates maintenance of a steady physiologic replacement.
Liothyronine
- Synthetic L-T3.
- More difficult to monitor than T4.
- More expensive.
- Shorter half-life.
- Treatment of choice for Myxedema coma.
- Short term suppression of TSH.
- Greater risk of cardiotoxicity.
Liotrix
- Combination of levothyroxine and liothyronine.
- Ratio of 4:1.
- No advantage over levothyroxine so not frequently used.
Uses
- Cretinism –congenital hypothyroidism
- Adult Hypothyroidism
- Myxoedema coma
- Non-Toxic Goiter
- Thyroid Nodule
- Papillary Carcinoma of Thyroid
Adverse reactions
- Hyperthyroidism (or symptoms of hyperthyroidism).
- Cardiovascular toxicity (tachyarrhythmias, angina, and infarction)
- CNS stimulation
- Insomnia.
Classification of Antithyroid drugs
Inhibit thyroid hormone synthesis (Thioamides)
- Propylthiouracil,
- Methimazole,
- Carbimazole
Inhibit iodide trapping [Ionic inhibitors]
- Thiocyanate,
- Perchlorates,
- Pertechnetate
Inhibit hormone release
- Iodides,
- Lithium
Destroy thyroid tissue
Radioactive Iodine
Inhibit peripheral conversion of T4 to T3
- Amiodarone
- β-blockers
- Corticosteroids
- Propylthiouracil
- Ipodate
Thioamides
- Propyithiouracil
- methimazole,
- carbimazole.
- Inhibit the peroxidase enzymes catalyzing the oxidation of iodide, iodination of thyroglbulin
- Inhibit coupling reaction
- PTU also inhibits the peripheral deiodination of T4 to T3. Do not block uptake of iodine by gland.
- Delay in absorption
- Delay in onset 3-4 weeks, because formed T4 takes time to deplete, only further formation is stopped.
Pharmacokinetics
Propyl thiouracil
- PTU is readily absorbed
- Bioavailability is 50-80%
- Volume of distribution is equal to total body water
- Drug accumulates in thyroid gland
- Secreted though kidneys, glucuronide form within 24 hours of administration.
- Half life in plasma is 1.5 hours (90 minutes)
Methimazole,
- Completely absorbed after oral administration
- Accumulates in thyroid
- Half life is 6 hours
- Volume of distribution is equal to that of PTU, but excretion is slower.
Both drugs cross placenta. In pregnancy PTU is preferred, minimum dose required is given.
Methimazole causes congenital abnormality in fetus. Both drugs are excreted in breast milk in small quantity, but safe for nursing infants.
Uses
- Used for control of hyperthyroidism until surgery.
- Suppression of thyroid hormone synthesis until the effect of radioactive iodide begins.
- Long-term therapy of mild-to-moderate hyperthyroidism.
- The drugs are given orally.
Adverse effects
a. Mild maculopapular rash,
b. joint pain,
c. headache,
d. nausea,
e. loss of hair,
f. altered sense of taste or smell,
g. Hepatitis,
h. Cholestatic jaundice
i. Rare: agranulocytosis(0.1-0.5%) –most serious but not common, leading to leukopenia, sore throat, upper respiratory tract infection, immediately stop treatment.
j. Crosses the placenta and enters breast milk, which can lead to hypothyroidism in the fetus and nursing infant.
Differences
| Propylthiouracil | Carbimazole |
| Less potent | 10 times more potent |
| Highly PPB | Less bound |
| Less transfer across placenta & milk | Crosses the placenta |
| Half-life=1.5 hrs | 6-10 hrs |
| DOA=6-8hrs | 12-24hrs |
| No active metabolites | Active metabolites |
| Multiple doses | Once daily dose |
| Inhibits T3 conversion into T4 | Does not effect |
Iodides
- Prepared in 1940s, now rarely used as sole agent.
- Small amounts of iodine (75-100 ng/day) are required for hormone synthesis.
- But high concentrations (+ 50 mg/day) produce autoinhibition.
- lodides inhibit organification
- Inhibit release of thyroid hormones.
- Diminishes vascularity of the gland.
Uses
- Used only preoperatively to shrink the gland. (prior to surgical removal of the gland).
- Treatment of thyroid storm.
- Prophylaxis of endemic goiter.
- It is given as Lugol’s solution (iodine and potassium iodide).
- Effects are visible within 24 hours. It is no longer used in long-term therapy.
Adverse reactions
- Hypersensitivity reactions
- Drug fevers,
- Metallic taste,
- Bleeding disordes,
- Swollen salivary glands,
- Conjunctivitis,
- Rhinorrhea
- Gastric irritation.
Long-term use can lead to sudden disinhibition of hormone synthesis, producing acute hyperthyroidism.
Radioactive Iodine
- Given orally or I/V.
- Rapidly taken,absorbed,,concentrated by thyroid,incorprated into storage follicles.
- Leads to partial or total destruction of the gland by emission of beta particles.
- Damage to surrounding tissue is minimal.
- Metastatic carcinoma of thyroid
Advantages
- simple
- low cost,
- effective,
- easy administration,
- absence of pain,
- no surgical risk,
- no genetic damage.
Disadvantages
- Major: hypothyroidism.
- Long latent period of response.
- Not suitable for young patients.
- Should be avoided during pregnancy.
Iodinated Contrast Media
- Diatrizoate (PO), Iohexol (PO OR I/V).
- Inhibit conversion of T4 to T3 in liver,kidney,pituitary gland & brain.
- Useful adjunctive therapy in thyroid storm
- Alternatives to iodides or thioamides
Beta Blockers
- Excess thyroid hormones, upregulation of B-adrenergic receptors.
- Tachycardia, tremors, anxiety.
- Propranolol,metoprolol,atenolol.
- Inhibits peripheral conversion of T4 to T3
Thyroid Storm
Acute exacerbation of symptoms of disease thyrotoxicosis, if not treated quickly, leads to death
Treatment:
1. Supportive
Fever controlled by antipyretics, I/V fluids, etc.
2. Drug treatment
- Propanolol given I/V 1.2 mg after that orally 40-80 mg every 6 hours, if contraindicated, Diltiazem is used for CVS symptoms and severe tachycardia.
- Potassium Iodide (10 drops orally daily] –retard release of thyroid hormones from gland.
- Iodinated Contrast Media(1g orally)
- Hydrocortisone to prevent shock
- Antithyroid drugs to inhibit thyroid hormone synthesis.
- Supportive therapy
 howMed Know Yourself
howMed Know Yourself