Diabetes is diagnosed if:
a. HbA1C ≥ 6.5%, OR
b. Fasting plasma glucose (FPG) ≥ 126 mg/dl (7.0 mmol/l), OR
c. Two hour plasma glucose ≥ 200 mg/dl (11.1 mmol/l) during an OGTT, OR
d. A random plasma glucose ≥ 200 mg/dl (11.1 mmol/l)
*ADA guidelines
Recommendations: Detection and Diagnosis of Gestational Diabetes Mellitus
Screening: Use plasma glucose fasting and 2 hours after breakfast, if abnormal go for 50 gram oral glucose challenge test.
In pregnant women previously known to have diabetes, and screening test abnormal, go for confirmatory test for diagnosis of GDM at 24-28 weeks gestation, using a 100 gram glucose- OGTT .
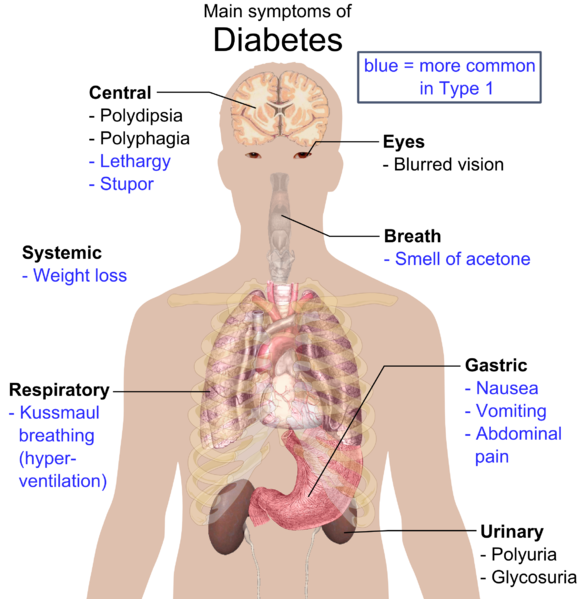
Complications of Diabetes Mellitus
Short- term Complications: (Metabolic)
1. Hypoglycemia:
Blood glucose level less than 3.0 mmol/L associated with non specific symptoms which are reversed by administration of glucose.
2. Diabetic Ketoacidosis:
It is complication of diabetes in which excessive formation of ketone bodies occurs, making the chemical balance of the body for more acidic.
Ketone bodies include:
- Acetoacetate
- B-Hydroxy Butyrate
- Acetone
Pathogenesis:
Uncontrolled diabetes leads to low insulin concentration, which in turn causes increased lipolysis and free fatty acid synthesis. This leads to increased fatty acid oxidation in liver and increased hepatic ketone formation and decreased peripheral tissue metabolism of ketones causing ketonemia and ketonuria leading to acidosis.
3. Non Ketotic hyperosmolar diabetic coma:
Hyperglycemic coma without ketosis.
Pathogenesis:
Sufficient insulin is present to prevent hepatic ketogenesis but insufficient to prevent severe hyperglycemia, which causes increased extracellular osmolality and extensive water loss.
Due to hypersomolality, patient undergoes mental confusion and becomes unable to respond to thirst to replace water leading to dehydration.
4. Lactic acidosis:
It may occur in
- Hypoxic conditions e.g. decreased oxygenation, hypovolemia(shock)
- Metabolic disease e.g. diabetes, liver disease.
- Drugs/toxins e.g. ethanol, salicylates.
- Inborn errors of metabolism: Resulting in low pH and high lactate levels in blood .
Long term complications:
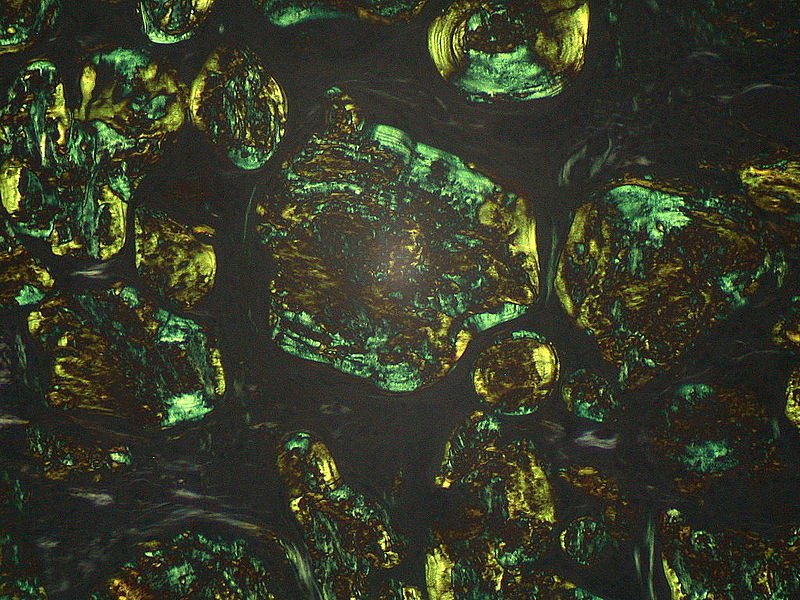
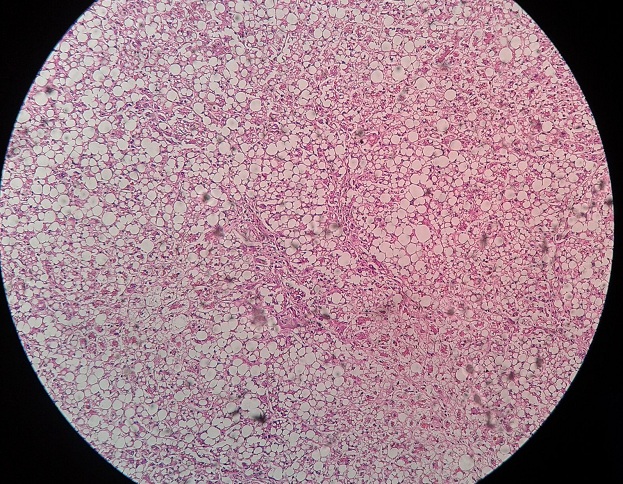
Microangiopathy
Pathogenesis of microangiopathy
- Long standing diabetes
- Combination of glucose with proteins – Particularly collagen in blood vessels – Glycosylation.
- Excess deposition of glycosylated type IV collagen in the basement membrane
- Thick and Leaky blood vessels.
- Chronic Ischemia & protein loss into tissues.
- Organ damage…
- Proposed mechanisms
- Hyperglycaemia- stimulates aldol reductase enzymes – metabolise glucose to sorbitol (polyol sugar) – tissue accumulation
- Non-enzymatic glycation of proteins (Amadori products, ‘ advanced glycation endproducts’)
Atherosclerotic diseases
- Atherosclerosis:
– Increased incidence of strokes, CAD , and peripheral vascular disease
– Acute Ml is the most common cause of death
- Hyaline arteriolosclerosis
- Diabetic microangiopathy
Nephropathy
- Renal failure due to nodular glomerulosclerosis
- Renal papillary necrosis
Ocular disorders
- Increased risk for cataracts and glaucoma
- Retinopathy (15%):
- Nonproliferative: microaneurysm formalion; flame hemorrhages; exudates
- Proliferative: formation of new vessels (neovascularization); increased risk for retinal
- Detachment and blindness; annual ophthalmologic examination is mandatory
Peripheral nerve disorders
- Diabetes mellitus is the most common cause of peripheral neuropathy
- occurs in 70-80%
- Sensory: paresthesias: patients complain of burning feet
- Motor dysfunction; muscle weakness; decreased deep tendon reflexes
- Neuropathy is the most important risk factor for pressure ulcers on the bottom of the feet (patient cannot feel pain)
Autonomic nervous system disorders
- Autonomic neuropathy: gastroparesis (delayed emptying of stomach);
- Impotence;
- Neurogenic bladder;
- Orthostatic hypotension
Cranial nerve (CN) disorders
- Diabetes is the most common cause of multiple cranial nerve palsies
- Cranial nerves (CN) most often involved: CN lll, IV and VI
Skin disorders
- Necrobiosis lipoidica diabeticorum: well-demarcated yellow plaques over the anterior surface of the legs/dorsum of ankles
- Lipoatrophy: atrophy at insulin injection sites due lo impure insulin
- Lipohypertrophy: Increased fat synthesis at Insulin Injection sites
Infectious disorders
- Urinary tract infections
- Candida Infections; e.g., vulvovaginitis
- Rhinocerebral mucormycosis: Producing infarction (vessel Invader) and abscesses
- Cutaneous infections: usually Staphylococcus aureus abscesses
Joint disorders
- Neuropathic joint: related to lack of sensation;
- Bone or joint deformity from repeated trauma
 howMed Know Yourself
howMed Know Yourself