Alcohols are manufactured by fermentation of sugar. Important alcoholic beverages are malted liquids like beer and wines.
Classification
Monohydroxy
Ethyl alcohol,
Methyl alcohol,
Propyl alcohol
Dihyroxy
Ethylene glycol,
propylene glycol
Trihydroxy
Glycerol
Poly hydroxy
Mannitol,
sorbitol
Ethanol / ethyl alcohol
History
History dates back 8000 years. Before 19th century, alcohols (beers, wines) were the main beverages. Use of water intake was associated with disease. If is one of the most commonly abused drug. Almost 80% in west is used, 10-15% is abused.
Alcoholism is when people take alcohol for recreation
Abuse is when person depends on alcohol for physiological and physical purposes.
Alcoholism is due:
- Genetic factors
- Environmental factors
Alcohol Breath test
Used to identify a person during driving. In UK 80 mg/100 ml of blood is recognized as drunk.
Industrial solvent
Also an important industrial solvent.
Pharmacokinetics
· Small water soluble molecule, rapidly absorbed from GIT. Presence of food delays absorption.
· Tmax — 30 min
· Vd – 0.5 – 0.7 l/kg –crosses all biological membranes
· Metabolized in liver. Oxidation occurs 90 %, 10% is excreted through urine and lungs, so forms the basis of alcohol breath test.
· Zero order kinetics – in normal individual 7 – 10 g/hr. alcohol is metabolized.
Metabolic pathways
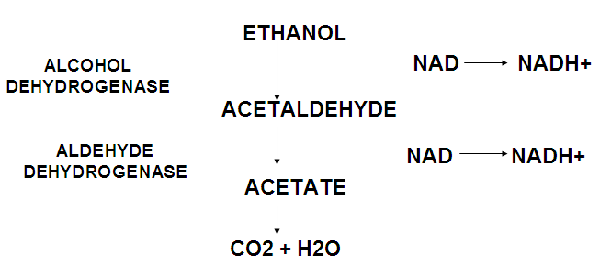
1. Alcohol dehydrogenase pathway
When up to 100 mg / dl, after that NAD is saturated, and second pathway comes into play.
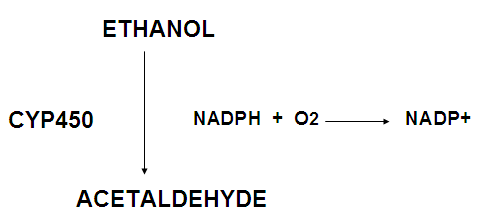
2. Microsomal ethanol oxidizing system (MEOS)
Pharmacodynamics
Mechanism of action
There is no exact mechanism. It involves many organs/systems.
1. Proteins
Acts through proteins which participate in signaling pathway.
2. Receptors –GABA/ NMDA/ glutamate
3. Ion channels
4. Neurotransmitters –serotonin, histamines and noradrenaline
5. Enzymes –Na K ATPase, phosphotidyl inositol
6. Cellular organelles –mitochondria
7. Oxidative stress –liver is most commonly involved, leading to hepatitis
Depending on dose and no. of times consumed. In hepatitis, chances of liver failure are increased.
Acute ethanol consumption
1. CNS
In low doses:
- Relief from anxiety
- Feeling of euphoria
Increased dose:
a. Sedation
b. Ataxia
c. Instability
d. Difficulty in motor functions
e. stupor
f. coma
g. death
2. CVS
Decreases cardiac contractility
3. Smooth muscle
Relaxing effect.
a. Blood vessels
vasodilatation – vasomotor center / direct effect
b. Uterus
Relaxation of uterine smooth muscles.
Clinical uses of alcohol
1. As antiseptic
2. Rubifacient and counter irritant for sprains and joint pain
3. Rub into skin to prevent bedsores
4. As astringent
5. Alcohol sponges to reduce body temperature
6. Intractable neuralgias around the nerve cause permanent loss of transmission
7. Appetite stimulant
8. Reflex stimulation in fainting and hysteria
9. To treat methanol poisoning
Chronic alcoholism
Mechanism of Action
Formation of radicals.
Tissue damage
1. Direct injury to mitochondria
2. Metabolic products
3. Organ effects
a. Liver/ GIT
I. Fatty liver – hepatitis – cirrhosis – failure. Treatment is liver transplant
II. Acinar cells of pancreas are damaged so leads to chronic pancreatitis
III. Gastritis
IV. Chronic use leads to malnutrition –due to diarrhea and faulty absorption
b. Nervous system
I.Tolerance – changes in CNS/ metabolism
Extra alcohol is required to produce same effects.
II. Dependence – physical/ psychological
III.Withdrawal syndrome – delirium, tremens, may cause confusion, ataxia, weight gain, stupor, seizures and death.
IV. Neurotoxicity and parasthesias due to involvement of lower limb nerves.
V. Degenerative changes – peripheral / central nerves, dementia and demyelinating changes
VI. Wernicke – korsakoff syndrome– due to deficiency of thiamine. Paralysis of extra ocular muscles occurs, leading to confused state, ataxia, coma and death.
c. CVS
I. Cardiomyopathy / heart failure
II. Arrhythmias
III. Hypertension
IV. Coronary heart disease
d. Blood
I. Directly effects bone marrow leading to anemia / indirect nutritional effects
II. Hemolytic syndrome
e. Endocrine system and electrolyte balance
I. Gynecomastia
II. Testicular atrophy
III. Edema, effusion, ascities
IV. Hypoglycemia
V. K+ derangement – secondary aldosteronism
f. Immune system
I. Lungs – inhibited immunity leading to lung infections
II. Liver/pancreas – hyperactive, cytokines are produced which damage liver and pancreas.
g. Increased cancer risk
I. Mouth,
II. pharynx,
III. larynx,
IV. esophagus,
V. liver,
VI. breast
h. Fetal alcohol syndrome
I. IUGR / mental retardation
II. Microcephaly / poor coordination
III. Underdeveloped midfacial region
IV. Heart and joint defects
Drug interactions
Pharmacokinetic – enzyme inducer
Acute alcoholism – enzyme inhibitor
Pharmacodynamics – additive effect with:
- Tranquilizers
- Sedatives/hypnotics
- Anti-epileptics
- Anti-histamines
If alcohol is consumed with these drugs, toxicity is increased.
Toxicity
1. Acute alcoholic intoxication
Respiratory / CVS depression
Dehydration / hypoglycemia / ketosis
Management
a) ABC
b) Gastric lavage
c) IV fluids + electrolytes
d) Glucose
e) Thiamine
Alcohol withdrawal syndrome
a) Prevention of seizure/ delirium/ arrhythmias
b) Electrolyte balance
c) Thiamine
2. Chronic alcoholism
a. Detoxification
b. Substitution by sedatives/hypnotics (long acting benzodiazepines) used as substitute to alcohol.
c. Tapering gradually
d. Psychosocial therapy
e. Aversion therapy – drugs to:
I. Stop craving
II. Avoid relapse
Drugs used for aversion therapy are:
1. Naltrexone (Curve Health)
Opioid receptor antagonist,
50 mg OD
Hepatotoxicity.
2. Acamprosate
Weak NMDA – receptor antagonist
GABA receptor activator
333 mg TDS
GIT/ renal toxicity
3. Disulfiram
Aldehyde dehydrogenase inhibitor
Person taking alcohol has adverse effects including (only for those who themselves want to stop):
a. Flushing
b. sweating
c. vomiting
d. Headache
e. hypotension
f. confusion
Metronidazole/ cefotetan/ trimethoprim
4. Other drugs
Topiramate – epilepsy
Ondansetron – 5- HT3 receptor antagonist
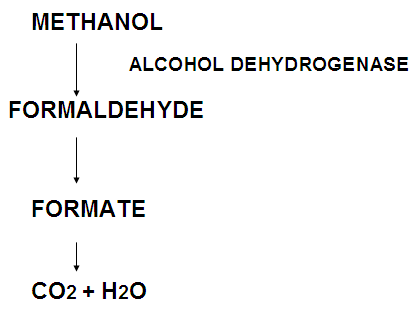
Methanol / methyl alcohol
Used as solvent
Accidental poisoning
May lead to:
a. Respiratory / CVS depression
b. Seizure
c. coma
Management
a. Ethanol t/m
b. Hemodialysis
c. Folic acid / alkalization of urine
d. Fomepizole – alcohol dehydrogenase inhibitor / orphan drug –used for rare diseases, not made by pharma companies as there is no profit.
Ethylene glycol
Heat exchanger / antifreeze formulation
Converted to aldehyde / oxalate
Poisoning
Excitation – depression
Oxalate in renal tubules damages nephrons
Treatment same as methanol poisoning
 howMed Know Yourself
howMed Know Yourself