Introduction
Barbiturates were used as sedative/hypnotic for a long time. Now non-preferred because of:
- Non-selective depression of CNS
- Low therapeutic index
- Drug interactions –enzyme inducer
- Cause dependence and tolerance
Less safer than benzodiazepines
Still have place in clinical applications.
- Thiopentone sodium is ultra short acting, used in induction anesthesia.
- Phenobarbitone is long acting, used as anticonvulsant and antiepileptic for tetanus, narcolepsy, etc.
Chemistry
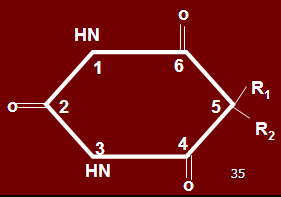
– Barbituric acid nucleus is essential, which has no sedative activity itself
– Urea + Malonic acid = barbituric acid.
– Weak acids
– Cross lipid membranes rapidly
Carbon 5 substitutions give rise to various barbiturates like aryl and alkyl groups, responsible for sedative activity.
Oxygen at position 2 substitution with sulphur forms thiobarbitone, becomes more lipid soluble, has increased duration of action, increased onset, increased degradation, increased hypnotic activity.
When desulfuration occurs, oxybarbitone is formed.
Pharmacokinetics
- Absorbed well orally. Difference in different formulations may occur.
- Onset of action is 10-60 minutes.
- Absorption is delayed, I/V route is used for management of status epilepticus and induction anesthesia.
- Bound to plasma proteins & compete for binding sites
- Metabolism varies
- In most cases oxidized by hepatic enzymes & cause Induction. Oxidation of radicals at position 5 is responsible for termination of activity of barbiturates.
- Opening of barbituric acid ring
- Thiobarbitone is converted into oxybarbitone by desulfuration
- Finally conjugated & excreted in urine.
- Cytochrome p450 is usually involved. Microsomal phase II glucuronyl transferrase is involved. Besides microsomal enzymes barbiturates may also induce delta aminolevulinic acid synthetase, leading to exacerbation of disease in patients suffering from porphyria.
- Can also increase their own metabolism, accounting in part for tolerance known as auto induction
- Most of the barbiturate metabolites are inactive pharmacologically.
- Long acting phenobarbitone has elimination t ½ = 5-6 days & accumulation can occur with multiple dosing.
- Barbiturates appear to increase the duration of opening of GABA gated channels.
Mechanism of Action
- Barbiturates bind with GABA component of receptor in neuronal membrane
- GABA A is pentameric structure having alpha, beta & gamma subunit.
- 16 genes, currently known to encode the 5 subunit of GABA A receptors
- GABA binds to α & β subunits to initiate gating of Cl- channels.
- Barbiturates do not bind benzodiazepine site, but have different sites. Action is similar to GABAergic opening of chloride channels, leading to hyperpolarization.
- Barbiturates appear to increase duration of opening of GABA – gated chloride channels. Although they are GABAergic but have separate binding site.
- At high concentrations, barbiturates are GABA – mimetic & directly activate Cl- channels.
- Also inhibit calcium dependent release of neurotransmitters
- Depress sodium and potassium channels in very high doses
- Barbiturates are less selective in their actions than benzodiazepines
- Barbiturates also depress the action of excitatory neurotransmitters and exert non-specific membrane stabilizing effects in parallel with their effects on GABA neurotransmission inducing full surgical anesthesia & respiratory depression. (Low margin of safety).
- Cause prolongation of total time of sleep. REM sleep and stage 3 and 4 are disrupted, may lead to rebound insomnia, nightmares, which may occur even after a single dose. Sleep cycle is disturbed, less satisfied sleep, hangovers and irritability occurs.
- Impair learning, short term memory, judgment, in psychoactive patients after a single dose may produce euphoria, allergic reactions.
Performance is impaired for 10-22 hours for purposes of driving, flying or handling machines
- Euphoria leads to dependence and hyper excitability.
- Within a few days (1-2 weeks) tolerance develops and dose has to be increased nearly 6 times for normal effects.
Pharmacological Actions
1. CNS
a. Sedation/hypnosis & anesthesia
– Can produce all degree of CNS depression
– Sedation/hypnosis – anesthesia – coma depending on dose
b. Effects on sleep
– Barbiturates decrease REM sleep & cause dream deprivation
– Elderly persons become confused, agitated & amnesic.
c. Anticonvulsant
– Very effective in higher dose
– Cause respiratory depression
There are chances of laryngeal spasm, coughing and hypoxic drives.
Laryngospasm is a complication of barbiturates, so no longer preferred when used as anesthetic.
Low doses
– Decrease low frequency activity (delta & theta wave)
– Increase low voltage fast action (electrical arousal of reticular formation)
– Accompanied by clouding of consciousness & euphoria.
High dose
– Large amplitude, random slow waves as appear in sleep observed & consciousness is lost
Much High dose
– Brief periods of electrical silence
d. Analgesia
– None
e. Effects on ANS
– Body temp decreases
– Blood pressure decreases
f. Neuromuscular Transmission
– Low dose – increase twitch response
– High dose – Blockade of NMJ
2. Respiration
– Decrease rate progressively
– Decrease drive with increasing dose
– Cough, sneezing, laryngospasm can occur with I/V admin.
3. CVS
– Myocardial depression with increasing dose.
– Arrhythmia & decreased B.P
Decreased cardiac contractility and reflex tachycardia
4. GIT
– Tone decrease
5. Liver
– Enzyme induction – increase metabolism of itself & other drugs metabolized by microsomal P450 (delta amino levulinic acid)
Interfere with endogenous steroids, corticosteroids and oral contraceptives.
6. Kidneys
– Decrease Na+ & glucose reabsorption – glycosuria & Natriuresis
Adverse Effects
1. CNS
Drowsiness,
Ataxia,
Amnesia,
Euphoria.
2. Respiration
Depression,
Hiccough,
Laryngospasm,
Bronchospasm
3. CVS
Decreased B.P—- Myocardial depression
4. Liver
Enzyme induction
Porphyria
5. Allergy
Facial edema,
Urticaria
Bullous eruptions
Drug automaticity
Automation occurs when barbiturates are taken by elderly. The sleep is less satisfying and they forget that they had taken the tablet, repeated night awakenings compel them to take another tablet, and thus they keep on increasing the dose. This may be fatal. They may become even more irritable.
Therapeutic Uses
1. Anticonvulsant in epilepsy & convulsant poisoning .
2. Used in psychoanalysis (abreaction) in psychiatry
3. Treatment of hyperbilirubinemia in neonates & kernicterus. Also in Criggler Najjar syndrome. They induce the enzymes which conjugate bilirubin.
4. Treatment of selective cases of cholestasis etc.
5. Used in anesthesia (ultra-short acting)
6. Dextroamphetamine dose adjustment
7. In hypnosedative withdrawal, although benzodiazepines are preferred, phenobarbitone is still used
8. In children, for per rectal administration of induction anesthesia, sedation (can give methohexitol)
9. Even in hepatic jaundice
10. Neopsychological procedures
Acute Barbiturate Poisoning
Signs & Symptoms
– Depressed respiration
– Coma
– Dilated pupils
– Decrease B.P
– Hypothermia
– cyanosis
Treatment
– O2 inhalation
– I/V line
– Dopamine
– Urine Alkalization
– Prevent renal failure
Drug Interactions
1. Potentiate other CNS depressant like benzodiazepines, alcohol, antihistamines etc.
2. Compete for plasma protein binding site with other drugs
3. Microsomal enzyme induction. Also induces mitochondrial enzyme aminolevulonic acid synthetase, so contraindicated in patients with porphyrias.
Continue Reading
Sedatives and Hypnotics -An Introduction
Flumazenil -Benzodiazepines Antagonist
Buspirone, Zolpidem, Zaleplon and other Sedative/Hypnotic Drugs
 howMed Know Yourself
howMed Know Yourself