Chloroquine is one of the oldest anti-malarial agent, effectively used in malarial infections. P. falciparum and vivax are the sensitive types.
It is a rapidly acting drug, targeting the asexual stage. It is an effective blood schizonticidal agent.
It is gametocidal, except for P. falciparum.
When administered, patient becomes afebrile within 24-48 hours. Use of chloroquine is declining recently due to the fact that most strains have become resistant. The mortality rate has increased along with the spread of malaria.
If after administration, afebrile stage is not achieved within 24-48 hours, it indicates specie is resistant and another drug should be used. There is very high resistance in some regions.
WHO recommends newer agents for combating infection.
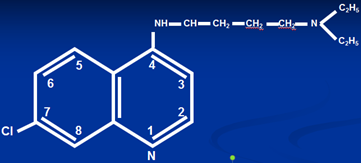
4 amino quinoline with quinoline nucleus.
Mechanism of action of chloroquine
- Entry into the parasitized RBCs
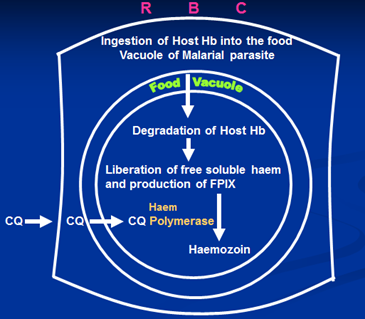
1. Accumulation in food vacuole of the parasite- role of pH gradient (chloroquine trapping)
Affects asexual cycle of plasmodium specie. Once administered, it has to enter site of action. It rapidly enters and gets concentrated in food vacuole, present within erythrocytes.
pH of food vacuole of plasmodium specie is acidic while chloroquine is a weak base, leading to change in pH of food vacuole. After entry, outer layer of food vacuole becomes water soluble (non-lipid soluble) so trapped inside food vacuole.
2. Hemozoin affinity for chloroquine
Plasmodium develops, multiplies and transforms by utilizing hemoglobin of human erythrocytes. It conserves hemoglobin, converting heme rapidly into insoluble and ineffective pigment known as ferri proto porphyrin 9 or Hemozoin, which is non-lethal and non-toxic to plasmodium speices. It has high affinity for chloroquine, which is another mechanism for trapping chloroquine.
Once trapped, chloroquine acts by one of many ways:
a. Inactivation of heme-polymerase responsible for conversion of heme part of hemoglobin into hemozoin. Conversion does not take place, heme is toxic to plasmodium, resulting in death of plasmodium.
b. Another way is that it enters and gets intercalated into DNA double helix held by weak hydrogen bonds connected strongly with covalent bonds, thus separation does not take place. Transcription, translation and multiplication is inhibited.
c. Impairment of metabolic process.
d. Damage to biological membranes
e. Inhibit DNA & RNA polymerase
f. Anti inflammatory role –
I. Inhibits phospholipase A2 (used rheumatoid arthritis), chemotaxis is decreased, resulting in decreased proliferation of antigen.
II. Trap free radicals
III. Also inhibit DNA and RNA response and synthesis
Uses
1. Main use is as anti-malarial. Highly effective for blood schizonticides. Mostly only sensitive for P. falciparum, as most strains are resistant now. Used usually to resolve febrile illness within 24-48 hours, if does not improve, then strain is resistant.
Problem of resistance is seen more commonly in South Asian and African belt. Resistance has developed in Afghanistan and Khyber Pathtunkhua. If we want to avoid relapse, Primaquine is used to eradicate tissue schizontal activity.
2. Previously used for chemoprophylaxis, now due to development of resistance, chloroquine is not used.
Other uses:
3. Anti-amoebic effect –infection caused by Entamoeba histolytica)
Amebic liver abscess (as chloroquine is concentrated in the liver) because:
- Lipid soluble
- Well distributed to all tissues
When administered, absorbed from upper part of small intestine, having activity against Entamoeba histolytica.
4. Anti-inflammatory
In autoimmune diseases e.g.
- Rheumatoid arthritis,
- Discoid Lupus Erythramatosus,
- Solar Urticria in those sensitive to UV light
Used for long time for rheumatoid arthritis, but because of associated ocular adverse effects, precaution is taken to have eye examination every 4 to 6 month to check retinal changes.
Hydroxy Chloroquine
More effective for long term treatment of rheumatoid arthritis as devoid of long term adverse drug reactions, especially eye changes.
Chloroquine – Resistance In Plasmodium Falciparum
With cholorquine there is emergence of resistance, which has limited its use. Primarily highly effective against febrile illness, relief is quickly achieved within 24 hours. It is easily available, well tolerated and cost effective but now uses are declining because of resistance.
1. Genetic Basis
Main mechanism, different genes have been discovered in plasmodium falciparum including gene type I and II.
2. Pfmdr-1, Pfmdr-2
3. CRTF
Another gene involved is chloroquine resistance transporter factor (CRTF)
4. Mutant heme polymerase
Not capable of converting heme into hemozoin.
5. Chloroquine is said to bind plasma protein P-glycoprotein related plasma protein related different genes.
6. Less concentration of chloroquine within food vacuole due to:
- Active efflux
- Reduced uptake
7. Pgh1
Reversal of resistance P-glycoprotein pathway verapamil, chlorpheniramine (antihistamine), disipramine.
Pharmacokinetics
- Given orally, I/M or by nasogastric tube in severely ill comatosed patients.
- If given by oral route, it is rapidly absorbed, well distributed and reaches most tissues of body including liver, spleen and kidneys, having high concentrations.
- Gets concentrated in erythrocytes, melanin containing tissues, hair, nails, eyes, retina and skin.
- PPP 60%, has high volume of distribution (about 3000 litres).
- High concentration of choroquine is achieved within plasmodium.
- Plasma half life is 1-3 days and terminal half life is 30-60 days. Trapped tissues slowly release indicating long terminal half life . metabolized by liver into metabolite in 2 steps:
- Converted into dysethyl choloquine, having terminal ethyl group.
- Another ethyl group is removed, metabolite called bis dys ethyl choloroquine.
- Metabolites are excreted by kidneys. Weak base so acidification of urine increases elimination.
- Administered by I/V route but when given I/V high plasma levels are achieved, with chances of toxicity esp. CNS and CVS –delayed cardiac condition, arrhythmias, cardiac arrest.
- Ideally given orally but I/M as well or nasogastric, also recommended, esp. in severely ill comatosed patients.
Dose
- Acute attack 600 mg base (4 tab.) then 300 mg after 6 h. then 150 mg bid for two more days.
- Add 100 mg proguanil/ day (2 tab.) in chloroquine-resistant area.
Chemoprophylaxis
No more recommended
- 300 mg base (2 tab.) / week,
- one week before entering the endemic area
- & 4 weeks after leaving.
Adverse Effects
Well tolerated in therapeutic range (600 mg) in divided doses, with no significant adverse effects. They include:
1. GIT:
- Anorexia,
- nausea,
- vomiting
- bitter taste
- local irritant effect:
2. CNS:
- Headache,
- confusion,
- psychosis,
- convulsions
- peripheral neuritis
3. CVS:
a. Hypotension,
b. T wave changes,
c. QRS widening
4. Skin: (esp. in rheumatoid arthritis)
a. Exfoliative dermatitis,
b. urticaria,
c. pruritus
Managed by epinephrine
5. Eye:
- Pigmentation macula
- Retinal artery stenosis
- Blurring of vision
- Visual field impairment
- Scotomas (hollows around eye)
- Colour perception impairment (even blindness)
When chloroquine or hydroxychloroquine are given for long term therapy, retina is examined whether changes have occurred or not.
6. Melanin containing tissues
Also deposited in melanin containing tissues resulting in:
- Hyperpigmentation of nails
- Pigmentation of skin
- Hair changes
7. Blood
- Hemolytic anemia especially in G6PD deficient patients.
- Leukopenia and thrombocytopenia have also been noted.
Contraindications:
On this basis chloroquine is contraindicated in patients suffering from:
- CNS disorders
- Psychoses
- G6PD deficiency
- Blood disorders
- Renal/hepatic failure
- CVS abnormalities
- Hypersensitivity (skin manifestations)
- Psoriasis (skin lesion)
As these conditions are aggravated.
Drugs Used in Chloroquine Resistant Malaria
Mono Drug Therapy
- Quinine
- Mefloquine
- Artemether
Combination Therapy
- Artemether 20 mg + Lumefantrine 120 mg (CoArtem) –highly recommended by WHO for uncomplicated malaria
- Pyrimethamine 25 mg + Sulfadoxine 500 mg (fansidar, malarest, malidar) –previously effective against falciparum malaria, now resistance has appeared, although some sensitivity, most strains are resistant
- Pyrimethamine 25 mg + Sulfadoxine 500 mg + Mefloquine 500 mg (fansimef) –single administration, withdrawn because of cardiovascular effects
- Pyrimethamine 25 mg + dapsone (maloprim )
- Quinine + doxycycline/ tetracycline
- Sulfadiazine + pyrimethamine + quinine
- Dapsone + chlorproguanil (lap dap)
- Atovaquone + proguanil (malarone)
Continue Reading
Artemisinin, Lumefantrine, Mefloquine, Primaquine, Atovaquone, Proguanil and Pyrimethamine
 howMed Know Yourself
howMed Know Yourself