Quinolones are the synthetic anti-microbial drugs.
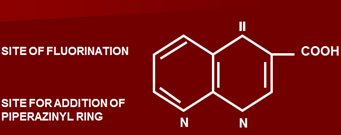
Structure of quinolones
Contain quinalene nucleus. Two main groups are present:
- Compounds having fluorine –fluorinated compounds
- Compounds not having fluorine –non-fluorinated compounds
Compounds which are non-fluorinated have a narrow spectrum, they have only carboxylic acid group at position 3.
Compounds which are fluorinated have fluorine at position 6. Also addition of piperazinyl ring at postion 7 occurs. Due to addition of these two complexes, an increase in anti-bacterial spectrum takes place.
Piperazinyl ring increases lipid solubility.
Anti-bacterial Spectrum:
Divided into four groups.
a. Oldest compounds
Active only against gram negative bacteria having a narrow spectrum. They are not fluorinated.
b. 2nd, 3rd and 4th group are fluorinated having wider anti-bacterial spectrum.
| First Generation | Spectrum |
|
|
| Second Generation | Spectrum | |
|
(less active against gram positive)
|
|
| Third Generation | ||
|
More active against gram positive including S. Pneumoniae | |
| Fourth Generation | ||
|
Additional activity against anaerobes | |
Mechanism of Action
Bactericidal action.
Enter bacterial cells passively through pores in cell membrane. Main action is by inhibition of two enzymes:
- Topoisomerase 2 –DNA gyrase enzyme
- Topoisomerase 4
Topoisomerase 2
- Responsible for opening of DNA strands during transcription or RNA formation
- Opening of DNA strand during replication
- Coiling and super-coiling of rapidly forming DNA molecule
Topoisomerase 4
- Causes separation of daughter chromosomes during replication.
- Death of cells occur, as all processes are blocked, producing bactericidal action.
- Human cells are less affected, as have certain different types of topoisomerases 1 and 3.
Mechanism of Resistance
Resistance is slow to occur against these drugs. Main reason is that they also cause disappearance of plasmid from bacterial cells, which is responsible for transfer of resistance against anti-microbial agents.
Thus, main mode of resistance is through chromosome, by:
- Cause alteration of a-subunit of DNA gyrase enzyme.
- Cause decrease in permeability of drugs in bacteria
- There are efflux mechanisms, pushing drug outside of bacterial cells.
Resistance is more common and rapidly develops against certain micro-organisms:
- Pseudomonas
- Gram positive organisms
- Neisseria species
- E. coli
- Enterobacter
- Campylobacter
Pharmacokinetics
- Well absorbed after oral administration, antacids, iron and zinc compounds delay absorption.
- Food interferes with absorption. Given 1-2 hours after meal.
- Onset of peak effect occurs after 1-3 hours.
- Distribution occurs to all body compartments well, except CNS where penetration is low.
- Only one drug Ofloxain has 90% penetration in CNS, others have less,especially if meninges are normal.
- PPB ranges between 10-40%.
- Nalidixic acid has 90%.
- Fluronited compounds have only 10-40%.
- Most quinolones are exceted in urine, up to 100-500 mcg/ml in urine, thus very effective in treatment of UTI.
- Some amount is metabolized in liver and excreted through bile.
- Moxifloxacin is totally metabolized in liver and excreted in bile, others are mainly excreted in urine, some 30-50% of these are also metabolized in liver.
- Nalidixic acid also has active metabolite hydroxyl nalidixic acid.
- Half life is between 3-8 hours.
Uses of Quinolones
First Generation
Have narrow spectrum, mainly used in:
- Uncomplicated resistant UTI
- Resistant cases of bacillary dysentery
Second, third and fourth Generation
Used in special situations mostly in resistant infections
1. Respiratory tract infections
- Bronchitis
- Sinusitis
- Otitis media
- Also used in atypical pneumonia
- Resistant cases of pulmonary tuberculosis (as 2nd line drug)
2. Complicated UTI (pseudomonas)
3. Also used in treatment of pyelonephritis/cystitis
4. Resistant cases of Gonorrhoea (penicillins are 1st line)
5. GIT infections, 1st line in treatment of:
- Enteric/typhoid fever,
- Bacillary dysentery,
- Cholera,
- Traveller’s diarrhoea
6. Bone (osteomyelitis), joint, soft tissues (cellulitis) and muscle infections
7. Anthrax caused by bacillus anthracis
8. Plague (Yersinia pestis)
9. Gram negative septicaemias
10. Neutropenic patients (immunocompromised)
11. Tuberculosis (2nd line) (also effective against atypical mycobacteria)
12. Chlamydial infections esp. of eye
13. Diabetic foot (in combination with clindamycin, as quinolones are active against gram negative organisms and clindamycin against gram positive) as there are increased chances of damage to foot due to neuropathy.
Adverse Effects
1. GIT
- Anorexia
- Nausea
- Vomiting
- Diarrhea
- Superinfections (pseudomembranous colitis, overgrowth of gram positive organisms)
2. Allergic Reactions
- Pruritis
- Articaria
- Skin rash
- Photosensitivity
3. Blood Dyscrasias
- Leukopoenia
- Thrombocytopenia
- Hemolytic anemia in patients of G6PD deficiency
4. CNS
- Drowsiness
- Vertigo
- Headache
- Myalgias
- Parasthesias
- In patients suffering from CNS disorders, may cause convulsions like patients of cardiovascular accidents, epilepsy, Parkinson’s disease.
- Cause convulsions in children in high doses.
5. Hepatotoxicity (Trovofloxacin)
6. Prolongation of QT interval esp. those of cardiac arrhythmias (Sparfloxacin & Moxifloxacin)
7. Achilles tendon rupture
Drug Interactions
2nd generation especially fluorinated compounds inhibit metabolism of certain drugs:
Increased plasma levels of these.
Contraindications
- Not given in pregnancy
- Neonates and small children as interferes with growth of epiphyseal cartilage
- Patients with renal insufficiency as excreted in urine
Dose
- Nalidixic acid 1 gram 4 times daily
- Pipemidic acid 400 mg twice daily
- Ciprofloxacin 250-500 mg twice daily
- Norfloxacin 400 mg twice daily
All are given for 7-10 days, if treatment is continued beyond 2 weeks, renal functions, LFTs and blood counts are done (hemolytic anemia, leukopoenia).
 howMed Know Yourself
howMed Know Yourself