Tetracyclines are a group of broad spectrum antibiotics whose general usefulness has been reduced with the onset of bacterial resistance. Despite this they remain the treatment of choice for some specific indications.
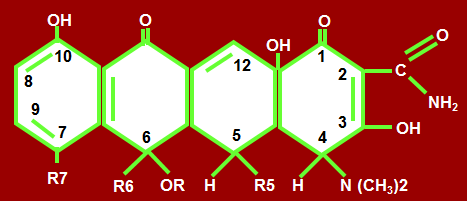
- They are so named for their four (tetra) hydrocaborn rings.
- Derivatives of Polycyclic Naphthacene Carboxamide.
- Reserved for only some infections due to wide spread resistance.
Classification Based On Source
1st natural tetracycline is Chlortetracycline obtained from Streptomyces Aureofaciens. Oxytetracycline is obtained from Streptomyces Rimosus
Natural
- Chlortetraycline
- Tetracycline
- Oxytetracycline
- Demeclocyline
Semi Synthetic
- Minocyclin
- Doxycycline
- Methacycline
- Lymecycline
- Clomocycline
- Rolicycline
Classification According to Duration of Action
Short acting (t ½ 6-9 hrs)
- Tetracycline,
- Oxytetracycline,
- Chlortetracycline
Intermediate acting (t ½ up to 16 hrs)
- Demeclocycline,
- Methacycline
- Clomocycline,
- Lymecycline
Long acting ( t ½ 17-20 hrs )
- Doxycycline,
- Minocycline (sensitive, still used widely)
- Glycyclines
- Tigecyclines –given I/V, action remains for 24 hours, microorganisms resistant to other drugs are still sensitive to these. There is difference is development of resistance. Efflux pumps are not involved, resistance is only plasmid mediated. These are newer drugs, given in life threatening septicemia.
Routes of administration
- Ointments
- Syrups
- I/V but not I/M due to:
- Pain
- Less soluble
Given as salts to improve solubility and absorption
Antibacterial spectrum of Tetracyclines
Broad spectrum, effective against broad range of gram positive and negative bacteria.
- Meningococi,
- Gonococi,
- Streptococi,
- Staphylococi,
- Pneumococi,
- H. influenzae,
- Rickettsia,
- Coxiella,
- Burnetii,
- Chlamydia spp
- Legionella spp,
- Ureaplasma,
- Mycoplasma pneumoniae,
- Atypical mycobacteria,
- Nesseria meningitidis,
- Vibrio cholerae
- Campylobater jejuni,
- Yersiniapestis,
- Francisella tularensis,
- Plasmodium spp.,
- Entamoeba histolytica,
- Anaerobes e.g bacteroides spp,
- Spirochetes -Treponema pallidum.
Mode of action
- Tetracyclines are bacteriostatic
- Inhibit protein synthesis by binding reversibly with 30S ribosomal subunits
- Interaction between amino acyl transfer RNA complex and mRNA ribosomal complex is inhibited.
- Amino acids are not added to the peptide chain
When administered, they reach site of action by 2 phases:
- Cross outer membrane of bacteria by passive diffusion and reach cytoplasm
- By active energy dependent process with involvement of carrier protein they enter the bacterial cell and block the combination
This active transport does not occur in human host cells thus devoid of action of antibiotics.
Additive action
It also prevents glucose utilization in bacteria. Oxidative phosphorylation is inhibited, thus energy production is inhibited.
Pharmacokinetics
- Administered orally, adequately but incompletely absorbed from GIT (stomach and upper part of small intestine)
- Doxcycline and minocycline 95-100% absorbed
- Tigecycline poorly absorbed administered I/V
- Plasma protein binding is variable; 70-80% Doxycycline and 30 -40% chlortetracycline
- Doxycycline enter paranasal sinuses
- Minocycline enters and secreted in tears & saliva. It is given to prevent carrier state but because of side effects not commonly used. In community acquired epidemics, it can be used.
- Widely distributed but cannot cross blood brain barrier, cross placenta except doxycycline and minocycline
- Secreted in milk of nursing mothers
- Mainly excreted through kidneys
- Doxycycline undergoes enterohepatic circulation and is secreted through bile in FECES, thus can be given in renal problems, as has non-renal excretion
- Rest of drugs may not cause pseudomembranous colitis. Some unabsorbed drug reaches colon, superinfection causing organisms flourish leading to pseydomembranous colitis. As complete absorption of doxycycline occurs, it does not go into colon in required concentration, chances of pseudomembranous colitis are increased with doxycycline.
Factors that affect oral absorption of tetracycline
- Tetracyclines have chelating property and form insoluble and unabsorbable complexes with Ca, Mg, Fe & Al
- Milk, antacids reduce the absorption of tetracyclines
- Food can reduce the absorption of all tetracycline except minocycline and doxycycline.
Therapeutic uses of tetracyclines
Drug of First Choice
- Rickettsial infections –Typhus, Rocky mountain spotted fever, Q fever
- Mycoplasma infection– atypical pneumonia
- Chlamydia Infections:
a. Trachoma and inclusion conjunctivitis
b. Ophthalmia neonatorum caused by Ch. Oculogenitalis (neoborn) - Venereal Diseases:
a. Syphilis in patients allergic to penicillin
b. Non Specific urethritis, endocervicitis due to Ch. Trachomatis
c. Granuloma inguinale, doxycycline is used - Brucellosis –with aminoglycosides and others.
- Bacillary infections including cholera, traveler’s diarrhoea.
- Replapsing fever
Drug of Second Choice
- Tetanus, anthrax, actinomycosis, listeria infection
- Gonorrhea in patients allergic to penicillin and cephalosporins
- Chancroid, E. Coli infection
Other infections and uses
- Amoebiasis along with other drugs
- Acne -6 month treatment, penetrate sebaceous glands
- COPD
- Prophylaxis of meningococcal meningitis during an epidemic minocycline
- Chronic hyponatremia due to inappropriate secretion of antidiurretic hormone, demeclocycline is used, because it renders the renal tubular cells unresponsive to ADH hormone
Side Effects Of Tetracyclines
1. Effect on calcified tissues. i.e teeth & bones.
If given to pregnant women deposited in fetal bones and by process of chelation tetra calcium orthophosphate complex is formed, which is deposited in bones development of bone suffers with short legs.
2. If given to infants and children under 12, yellow fluorescence followed by brown discoloration. Bone defects occurs of limbs. In teeth enamel hypoplasia, primary dentition suffers and pits are formed in teeth and great incidence of caries in teeth.
3. Irritation – epigastric distress, nausea, vomiting, diarrhea.
4. Superinfection (Candida, staph)-Psuedomembranous colitis
5. Fe, Al, Ca, Mg etc are chelated insoluble complexes formed, which are not absorbed.
6. GIT side effects due to two reasons:
Reach colon & suppress flora, vacuum is created and opportunistic organisms like Clostridia, resistant to drug start flourishing, mucosal layers are affected (Mucous shreds, neutrophil & diarrhea). It is due to toxins produced by them. Esp clostridium difficile causes damage to mucosa.
This situation can be life threatening, it is treated by administering vancymycin and metronidazole.
7. If given to patient of renal dysfunction, aggravate uremia because of catabolic effect on proteins (they increase load of N)
8. Outdated tetracyclines given are decomposed to epianhydro tetrayclines responsible for fancony like syndrome. Characterized by:
- polyuria,
- proteinuria,
- aminoacid urea,
- polydypsia,
- nausea
- vomiting.
9. Hypersensitivity reactions due to topical use. (dermatitis, morbiliform rash=),
10. Minocycline causes vestibular toxicity, nausea, vomiting dizziness, vertigo & ataxia.
11. Photosensitivity by demeclocycline & doxycycline
12. Ototoxicity, nephrotoxicity, hepatotoxicity.
13. Nephrogenic diabetes insipidus occurs with demeclocycline, this effect has been used for the treatment of chronic inappropriate secretion of antidiuretic hormone. (thus side effect is exploited)
Contraindications of tetracycline
- Renal impairment,
- hepatic insufficiency,
- pregnancy and lactation
- children under 8 years of age
- Do not use expired drugs
- Do not mix injectable with penicillin. Do not inject intrathecally
- Avoid in patients on diuretics as they increase blood urea.
Doxycycline
- To treat prostatitis, sinusitis, syphilis, chlamydia, pelvic inflammatory disease and acne rosacea
- Prophylatic treatment for infection by bacillus anthracis.
- Effective against Yersinia pestis, the infectious agent of bubonic plague
- Also used for malarial treatment and prophylaxis
- Elephantiasis disease cause by nematode (Wuchereria bancrofti)
 howMed Know Yourself
howMed Know Yourself