Adrenal hormones are released from the adrenal gland, which is divided into two parts:
- Adrenal cortex –hormones secreted are known as corticosteroids
- Adrenal medulla –hormones secreted are known as catecholamines
Anatomically adrenal cortex has three parts or layers:
- Zona glomerulosa –outermost concerned with secretion of aldosterone (mineralocorticoids)
- Zona fasciculate –secretion of glucocorticoids
- Zona reticularis –secretion of androgens
Regulation of Corticosteroids Secretion
Regulation is by two mechanisms:
- Negative feed back
- Positive feed back
Glucocorticoids (cortisol) production/secretion is regulated by negative feedback.
Mechanism
Mineralocorticoid (aldosterone) secretion regulation is by positive feedback.
Increased sympathetic activity leads to increased renin which increases aldosterone, resulting in salt and water retention
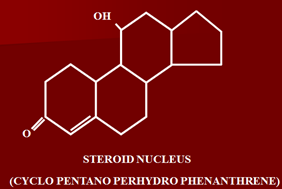
Chemistry
Steroids are chemically having large cyclopentanoperhydrophenanthrene nucleus.
Classification
Glucocorticoids
Natural
- Cortisol
- Cortisone
Synthetic
- Betamethasone
- Dexamethasone
- Prednisolone
- Triamicinolone
- Prednisone
- Methylprednisolone
Mineralocorticoids
Natural
- Aldosterone
- Desoxycorticosterone acetate (DOCA)
- Corticosterone
Synthetic
- Fludrocortisone
Glucocorticoids (According to Duration of action)
1. Short Acting (T ½ 8-12 Hrs)
- Cortisone –prodrug, converted in liver to cortisol/hydrocortisol
- Cortisol
2. Intermediate Acting (T ½ 12-36 Hrs)
- Prednisolone –very less mineralocorticoid activity as compared to cortisol
- Methylprednisolone –same effects as prednisolone except given by I/V route of administration
- Triamcinolone –has no mineralocorticoid activity
3. Long Acting (T ½ 36-72 Hrs)
- Paramethasone
- Betamethasone
- Dexamethasone -very potent anti-inflammatory activity
Glucocorticoids Administered by Inhalation– used in bronchial asthma
- Beclomethasone
- Budesonide
- Fluticasone
- Triamcinolone
- Mometasone
Steroids -Mechanism of Action
All steroids have the same mechanism of action, but differ in production of ultimate proteins.
- Crossing cell membrane
All steroids enter cell passively.
- Binding with cytosolic receptor
Mainly present intracellularly. Two types of receptors are involved:
- GR –alpha
- GR –beta
(GR = glucocorticoid receptor)
Receptors are distributed throughout the body. Mineralocorticoid receptors are present mainly in excretory organs like kidneys, colon and sweat glands, etc.
Receptors of glucocorticoids are present all over body.
- Dissociation of receptor from Hsp 90 & 70
Normally receptors are covered by regulatory proteins, which are of two types:
- HSP-90
- HSP-70
These are the heat shock proteins, the regulatory and stabilizing proteins. When steroids bind the receptors, they cause displacement of stabilizing proteins from receptor sites.
- Active transport of steroid-receptor complex into the nucleus
- Binding of activated receptor with DNA
Receptor separates and steroid binds DNA
- DNA transcripts the formation of specific mRNA
- Formation of specific protein lipocortin (Annexin 1)
mRNA enters cytoplasm and goes to ribosomes to bind them causing formation of specific proteins by the power of translation.
- Lipocortin (protein) inhibits phospholipase A2
Phospholipase is responsible for generation of arachidonic acid.
- Inhibition of formation of arachidonic acid from phospholipid
- Inhibition of formation of chemical mediators, including prostaglandins and leukotrines.
This is the anti-inflammatory mechanism of glucocorticoids.
Glucocorticoids Pharmacological Actions
Effects are divided into two main categories:
1. Metabolic Effects
a) Carbohydrate Metabolism
- Steroids in carbohydrate metabolism cause and increase in blood levels of glucose.
- Decrease utilization of glucose
- Cause increase in gluconeogenesis
- Cause increased breakdown of glycogen
All effects lead to increased glucose levels, producing diabetogenic effect.
b) Lipid Metabolism
- Lipolysis occurs
- In high doses, redistribution of fat to other parts of the body.
c) Protein Metabolism
- Have catabolic effect
- In high doses, cause loss of protein matrix from bones and cause thinning of skin and wasting of muscles
- Atrophy of skin, if applied topically
- Negative nitrogen balance
d) Water & Electrolyte Balance
Salt and water retention and excretion of potassium.
These effects are minor, in over dosage or prolonged use cause excretion of water
e) Excretion of urates
On prolonged administration, increase the chances of urine stone formation (urinary canaliculi)
f) Antivitamin D activity
Some anti-vitamin activity so cause increased excretion of calcium in urine.
g) Augment the action of growth hormone on adipocytes
(have specific lipase enzyme).
2. Non metabolic effects
a) Anti Inflammatory Action
Most important effect, causing reversal of all signs/symptoms of inflammation without removing cause. Thus have non-specific effect in inflammation.
b) Lympholytic action
Generalized decrease in lymphoid tissues in body occurs along with lymphocytopenia.
c) Immunosuppressive action
Cause a decrease in immunity by:
- Causing decrease in lymphocytes (decreased antibodies formation)
- Stabilization of mast cell membrane
- Due to anti-inflammatory effect
- Some anti-histaminic effect
d) Effects on Blood
- Cause increase in RBCs, hemoglobulin, neutrophils and platelets.
- Most important is that they cause decrease in eosinophils, decrease in basophils and monocytes, leading to anti-allergic effects
e) CNS
When patient starts taking steroids (in therapeutic doses):
- Elation occurs
- Increased appetite
- Euphoria
If taken in high doses, lead to:
- Insomnia
- Even psychotic behaviour
f) Decrease production of TSH & increased growth hormone production
Pharmacokinetics
- Natural steroids,
- After release bind specific proteins known as CBG (corticosteroid binding globulins)
- Metabolized in liver and excreted in urine
- Synthetic steroids can be given by various routes of administration:
- Oral route
- Topically
- Inhalation –bronchial asthma
- Parenteral
- Intra-articularly –rheumatoid arthritis
Therapeutic uses of Glucocorticoids
1. Replacement therapy in adrenal disorders
Very important logical use in
a. Acute adrenal insufficiency
Usually occurs when steroids are given in high doses for long periods and then abruptly stopped, due to negative feedback (availability of hormones), atrophy of adrenal gland occurs.
Treatment is to give hydrocortisone or cortisol 100-200 mg 6 hourly, until condition is controlled.
When giving steroids for long periods, dose is gradually tapered off.
b. Chronic adrenal insufficiency (Addison’s disease)
Due to tumor of adrenal cortex, infections (tuberculosis of adrenal gland) or removal, chronic insufficiency occurs.
Treatment is to give replacement therapy including glucocorticoids along with mineralocorticoids.
Cortisol in a dose of 20-30 mg, synthetic ones are given in equivalent doses.
Once patient is stabilized, two-thirds of the dose is given in the morning, while one-third in evening.
c. Congenital adrenal hyperplasia
Very rare congenital defect in synthesis of glucocorticoids, leading to excessive formation of androgens. This may be:
- Congenital
- Defect in last step of corticosteroid because of excessive enzyme responsible for synthesis
Androgens are formed one step earlier, especially in pregnant females virulization of female fetus occurs.
Treated by administering glucocorticoids.
2. Non-adrenal disorders (Empirical Uses)
Ist Line uses
- SLE and other Collagen disorder
Autoimmune disorders, very effective and live saving.
- Acute leukemias and lymphomas
In combination with anti-neoplastic drugs
- Status asthmaticus/Bronchial asthma
Hydrocortisone is given I/V 100-200 mg 6 hourly, until acute attack is controlled
- Gram negative septicemia
Life threatening condition, death may occur, given in combination with anti-microbial drugs.
- Cerebral edema
Medical emergency, may occur after head injury.
Dexamethasone is given for cerebral edema.
- Glomerulonephritis/Nephrotic syndrome
Affect especially membranous type of glomerulonephritis.
- Idiopathic thrombocytopenic purpura –sometimes repond to steroids
- Aplastic anemia
- Hemolytic anemia (acquired) –respond in emergency
- Immunosuppression
Used as immunosuppressive in:
- Rheumatoid arthritis
- Prevent transplant graft rejection
- Prevent graft vs. host reaction
- Auto immune thyroiditis
- Acute mountain sickness
In combination with acetazolamide and carbonic anhydrase inhibitors
Advantage of combination is that acetazolamide is that these have rapid action, while acetazolamide has delayed effects.
- Allergies
Especially seasonal (pollen)
- Acceleration of lung maturation in premature babies
Cortisol causes maturation of lungs and in premature infants, there is decreased release of cortisol so given to mother before delivery esp.
- Beclomethasone 48 hourly before delivery I/M.
- Again before 24 hours of delivery
15. Dermatologic conditions
- Contact dermatitis
- Lichen planus
- Pemphigus
- Seborrhoeic dermatitis
In most skin conditions steroids are used, esp. non-infective skin conditions.
16. Ocular conditions
- Acute conjunctivitis
- Choroiditis
- Uveitis
17. Diagnostic purpose
To access primary and secondary caused of Cushing disease (ACTH excess) give potent steroid, dexamethasone, if after administration decreased levels occur, patient has Cushing disease due to primary dysfunction of adrenal cortex.
If no effect is observed, ACTH excess is due to secondary causes (hyperpituitarism or ectopic production)
2nd/3rd Line uses
- Anaphylactic shock -1st line is adrenaline
- Ulcerative colitis
- Crohn’s disease
- Rheumatoid arthritis
- Osteoarthritis –non-responding
- Acute gout –when excessive swelling and pain occurs, along with NSAIDS and Colchicine
- Myasthenia gravis –along with neostigmine and physostigmine
- Aspiration syndrome –to avoid aspiration of gastric contents
- Bronchial asthma –along with other anti-asthmatics oral/inhalational
10. Acute spinal cord injury –to avoid inflammation and edema
Untoward effects of Glucocorticoids
1. Suppression of adrenal –pituitary axis
Prolonged administration caused negative feedback leading to atrophy of adrenal cortex. Steroids are not withdrawn abruptly, otherwise Addisonians crisis occurs. Dose is gradually tapered, to allow recovery time. Once axis is depressed, it may take months or even years to recover, but when given for short period in low doses (25 mg prednisolone daily for 5-10 days) there is no need to taper off dose.
2. Iatrogenic Cushing’s syndrome –in high doses
3. Hyperglycemia
Due to increased plasma glucose, effect on carbohydrate metabolism
4. Muscle wasting/myopathy
Catabolic effect on proteins
5. CVS
May cause retention of salt and water leading to:
- Edema
- Hypertension
- Even cardiac failure
6. Immunological
Anti-immunity effects, leading to decreased resistance to infections and delayed healing of wounds, making more prone to infections
7. Eye
- When used topically cause glaucoma on prolonged administration
- Posterior subcapsular cataract
- Corneal ulceration
8. GIT
a. May cause peptic ulcer, due to secretion of HCl and pepsin when taken orally for prolonged periods.
b. May aggravate ulceration,
c. In patients of peptic ulcer, may cause painless perforation
d. May cause increase in candidiasis of GIT
9. Bones
Due to loss of protein matrix may cause osteoporosis, leading to spontaneous fractures.
So patients taking steroids are advised to take calcium and vitamin D supplements to avoid.
10. CNS
In therapeutic doses:
- Euphoria
- Elation of mood
In excessive doses:
- Insomnia
- Psychotic behavior
- Aggravate psychosis esp. schizophrenia
- May cause increase in intracranial pressure on prolonged administration –although rare.
11. Growth suppression
Especially in children due to early closure of epiphysis
12. Hypokalemia
Due to retention of sodium and excretion of potassium. Danger is when patient is taking digoxin or diuretics.
13. Candidiasis
Usually in patients of bronchial asthma, taking steroids by inhalation, due to deposition of steroids in larynx, pharynx, leading to candidiasis.
In larynx ultimately laxity of vocal cords and hoarseness of voice.
- Nystatin mouth washes
- Azoles
- Amphotericin B mouth washes are used
- Acne & hirsutism
On prolonged administration, especially after topical use.
14. Striae and bruising –esp. when applied to skin
15. Miscellaneous
- Delayed wound healing –decreased immunity, delayed fibrosis
- Skin atrophy –loss of protein matrix
- Tendon rupture
- Menstrual disorders
- Thromboembolism
Contraindications
- Diabetes
- Glaucoma
- CVS disorders
- Hypertension
- Cardiac failure
Mineralocorticoids
Drugs causing increased sodium and water retention along with increased elimination of potassium, acting on the late distal part and collecting tubules.
Natural are not used in therapeutics.
Aldosterone hormone cannot be given orally because:
1. Has short duration of action
2. In older days, when it was used, it had to be given 5-7 times a day by I/M injection
Synthetic
Fludrocortisone in only used nowadays.
- Given about 5-7 times a week
- Can also be given orally
Use
- Treatment of adrenocortical insufficiency, replacement therapy in combination with glucocorticoids
- Treatment of hypotension esp. when due to excessive loss of sodium.
Dose
50-300 mcg daily. In children dose of 5 mcg/kg body weight daily by oral route of administration.
 howMed Know Yourself
howMed Know Yourself