It is the commonest endocrine disorder characterised by:-
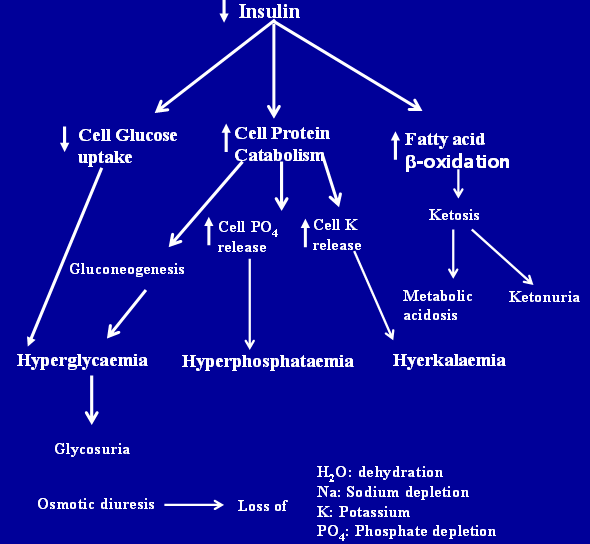
–Chronic hyperglycaemia
–Glycosuria
–Abnormalities of protein and fat metabolism
–Electrolyte disturbances
–Complications like degenerative changes of blood vessels
Diabetes Mellitus is a group of metabolic disorders of carbohydrate, protein and fat metabolism in which glucose is underutilized producing hyperglycaemia.
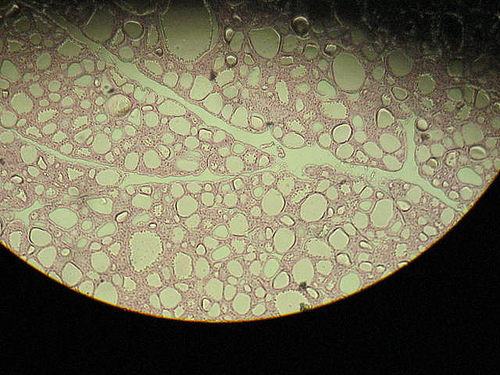
Photo by duisburgbunny
Classification of DM 1997
a.Type 1 diabetes
–Immune mediated
–Idiopathic
b. Type II diabetes
c. Other specific types of diabetes
d. Gestational diabetes mellitus
e. Impaired glucose tolerance
f. Impaired fasting glucose

Pathogenesis Of Type I– Diabetes Mellitus
• Cell mediated autoimmune destruction of the insulin secreting cells (b cells)
• Autoimmune process begins years before the development of diabetes mellitus
Antibodies
• Islet cell cytoplasmic antibodies 70-80% (sialoglycoconjugate antigen)
• Insulin antibodies 50% (autoantibodies)
Genetics
• Susceptibility to type I – inherited
• Mode of inheritance – complex, multigenic traits. MHC = c6. 11 loci on c9
• Concordance rate between identical twins-30%
• 95% whites with disease express hLA-DR 3 or DR 4 antigen
Environment
• Viruses – rubella, mumps, coxcackie, virus b.
• Chemicals
Pathogenesis Of Type II– Diabetes Mellitus
• Two major pathological defects
• Insulin Resistance
• Beta cell dysfunction
• Environment
• Diet – obesity – 60 – 80% diabetics
• Exercise – inverse relationship
• Loss of b cell function
• Loss of glucose induced insulin release
• (Selective glucose unresponsiveness)
• Disruption of normal pulsatile release of insulin
• Increased ratio of plasma proinsulin to insulin
• Insulin resistance
• Biological response to normal levels of circulating insulin
• Diabetogenes:
• Genetic factors contribute for diabetes mellitus type II
• Concordance rate in identical twins -100%
• 10% risk in an obese persons with a diabetic parent
• Mode of inheritance is unknown
• Multiple gene factors interact with exogenous influences
Causes Of Insulin Resistance
1. Abnormal b-cell secretion (pseudo-insulin resistance)
A. Familial hyperprinsulinaemia
B. Mutant insulin
2. Circulating insulin antagonists
A. Hormonal : catecholamines, glucagon, cortisol, growth hormone, thyroxine, estrogens, prolactin, AVP
B. Metabolities: non-esterfied fatty acids, ketone bodies, hydrogen ion
C. Immunological: anti-insulin antibodies, anti-insulin receptor antibodies
3. Changes in insulin receptors
A. Decreased number
B. Altered affinity
4. Post binding impairment
Screening
Individuals With High Risk Of D.M
• Strong family history
• Obesity / weight loss
• Women with previous h/o pregnancies leading to still birth, neonatal deaths, large newborn babies, toxaemia of pregnancy, obesity / family h/o diabetes
• Persons with any of the following clinical findings:
• Mental status e.g. fatigue, depression
• Skin manifestations e.g. Pruritis , vulvitis
• Balanitis, acne
• Eye manifestations: premature cataract,
• CVS findings
• Miscellaneous: neuropathy, muscle wasting
Screening
• US now recommends fasting plasma glucose in people > 45 years with 3 yearly follow-up
• Urine glucose used at present – only cost-justifiable pre-op test in otherwise healthy individuals < 45 years old
• Screening at younger ages recommended in high risk populations
Diagnosis
• Symptoms
– polyuria / polydypsia
– weight loss & fatigue
– recurrent infections
• “At Risk”
– pregnant / elderly / obese
– diabetogenic Rx e.g. glucocorticoids
– screening advocated for the over 45s
Gestational DM
• DM for first time in pregnancy
• Screening and diagnostic methods controversial
• No agreed WHO reference values
– Hatem M, et al. BMJ 1988; 296: 676-678
• proposed upper limits 2 h after 75 g glucose:
• second trimester: 7.5 mmol/L
• third trimester: 9.6 mmol/L
Need for close monitoring because of fetal risks
Secondary DM
• Pancreatic disease
– Ca pancreas, chronic pancreatitis, CF, pancreatectomy
– acromegaly, Cushing’s, aldosteronoma,
– phaeochromocytoma
• Drugs
– glucocorticoids, thyroxine,
– diuretics e.g thiazides
• Genetic
– Type 1 GSD, Down’s, Turner’s
Want a clearer concept, also see
 howMed Know Yourself
howMed Know Yourself