Maternal mortality is the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of duration and site of pregnancy from any cause related or aggravated by the pregnancy or its management and NOT due to any accidental or incidental cause.
Maternal Mortality Rate
Total number of female deaths due to complications of pregnancy, childbirth or within 42 days of delivery from puerperal causes in an area during a given year divided by total number of women of child bearing age (15-45 years).
Maternal Mortality Ratio
Total number of female deaths due to complications of pregnancy, childbirth or within 42 days of delivery from puerperal causes in an area during a given year divided by the total number of live births in the same area and year.
Risk Factors for Maternal Mortality
o Domestic Conditions
o Quality of Health Care
o Access to the Health Facility
o Physical, Economic, Social
o Availability of the Health Facility
o Manpower, working hours, physical
o Habits, Customs, Superstitions & other Cultural Patterns
o Nutritional Status of the mother
o Age of the mother
o Parity
o Repeated pregnancies
o Interval between two consecutive pregnancies
o Illiteracy
o Bad obstetric History
o Bad Medical History
Causes of Maternal Mortality
Direct Causes
o Hemorrhage
o Septicemia
o Toxemia( Eclampsia) of pregnancy
o Abortions
o Abnormalities of bony pelvis
o Ectopic Pregnancy
o Disproportion or malposition of fetus
o Improper management
o Poor technique in natal & postnatal periods.
Indirect Causes
o Anemia
o Infections & parasitic diseases
o Neoplasms
o Allergic, Endocrine, Metabolic , Nutritional Diseases
o Diseases of Blood
o Mental Disorder
o Disease of cardiovascular Sysytem
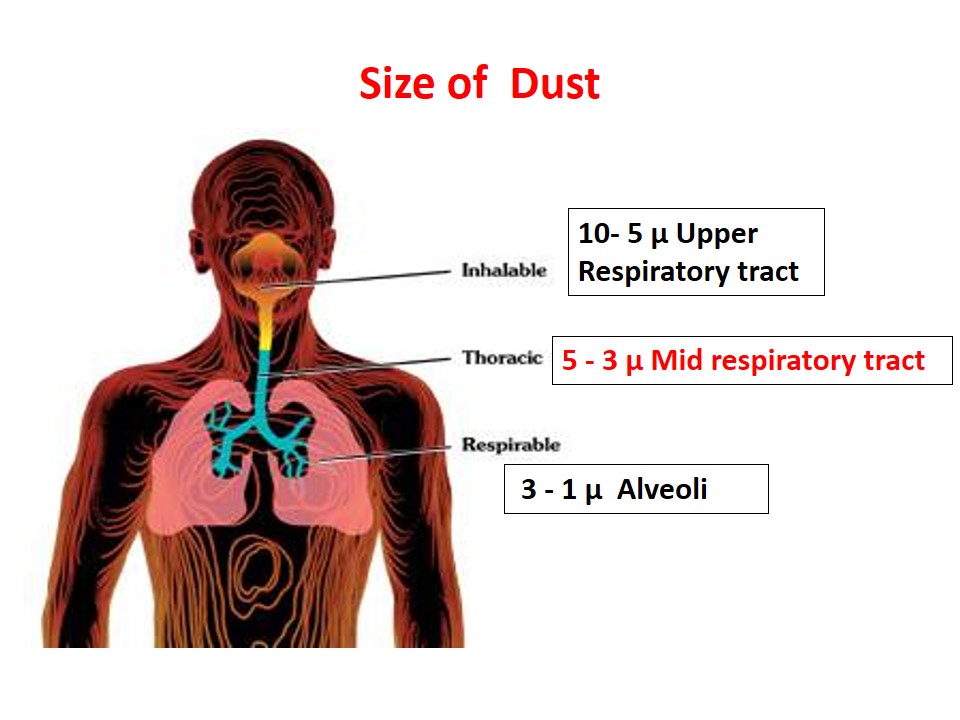
o Respiratory Disease
o Genito-urinary Diseases
o Disease of Bones & joints
o Chronic Poisoning
Prevention of Maternal Mortality
a) Pre – conception Guidance
b) Ante-natal / Pre-natal Care
c) Natal Care
d) Post-natal care
a) Pre-Conception Guidance
It means guiding women regarding her and her offspring care before she conceives. Guidance includes:
o Avoid medications
o Take folic acid (400 mcg) daily for at least one month before you conceive
o Eat a healthy diet and exercise in moderation
o Obtain necessary vaccinations ( rubella & chicken pox) at least three months before conception
o Identify and remove health hazards in your home or workplace
o Achieve a healthy weight
o Discontinue cigarettes, alcohol and other drugs
o Test for infectious diseases and screen for other medical problems
o Genetic counseling
b) Antenatal /Prenatal Care
Antenatal care
It means the care of mother during pregnancy.
Antenatal care aims at prevention and detection of problems of pregnancy at an early stage to reduce maternal and perinatal morbidity and mortality.
Schedule of Antenatal Visits
Ideally, a pregnant woman should be examined every month until 7 months of pregnancy, fortnightly (after 2 weeks) for the next six weeks, and weekly after that, if everything is normal.
However, this is difficult to achieve so a minimum of 3 antenatal visits should be aimed at as shown below:
- 1st visit at 20th week or as soon as the pregnancy is known.
- 2nd visit at 32nd week
- 3rd visit at 36 week
Antenatal /Prenatal care involves:
1. Routine antenatal care
2. Specific health Protection
3. Maternal continuous monitoring
4. Continuous monitoring of fetal development
5. Mental Preparation
6. Family Planning
i. Routine antenatal care
o History
o Physical Examination i.e. Height, weight blood pressure pulse, abdominal examination, etc.
o Investigations i.e. complete Blood Picture, Urine R/E, Blood group and Rh Factor, Random Blood Sugar, Ultrasound
o Prescribe Medications i.e. iron , folic acid, calcium
o Counseling i.e. nutrition, avoiding drugs, radiation, rest,
o Immunization
o Reschedule Next visit
Schedule of Tetenus Toxoid (WHO)
o TT1: At first contact or as early as possible during pregnancy
o TT2: Four weeks after TT1
o TT3: Six months after TT2
o TT4: One year after TT3
o TT5: One year after TT4 or during next pregnancy
Risk Approach in Pregnancy
Central purpose of antenatal care is to identify ‘High Risk’ cases as early as possible and give skilled care to them:
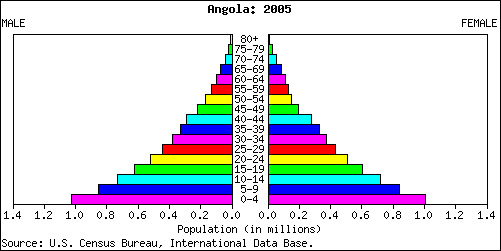
High-Risk Pregnancies
o Women less than 18 or more than 35 years of age.
o Short statured women (less than 5 feet tall).
o Grandmultiparae, i.e. those who have had 5 or more previous deliveries.
o Women delivering less than 2 years after the last confinement.
o Women with multiple pregnancy such as twins or triplets.
o Women with a history of complication in previous pregnancy such as hypertension, eclampsia, premature labor, difficult delivery, cesarean section (even if followed by a vaginal delivery), antepartum or postpartum hemorrhage, stillbirth or neonatal deaths.
o Women with medical problems such as anemia, hypertension, heart disease, diabetes, etc.
o Women with a malpresentation such as breech, oblique or transverse lie.
ii. Specific Health Protection in Pregnancy
o Anemia
o Other Nutritional Deficiencies
o Toxemia of pregnancy
o Tetanus
o Syphilis
o German measles
o Rh Status
o HIV infection
o Prenatal Genetic Counseling
iii. Continuous Monitoring of Maternal Well Being
o Routine check up
o Hypertension in pregnancy
o Gestational diabetes
o Pregnancy anemia
o Miscellaneous conditions
iv. Continuous Monitoring of Fetal Development
a. Abdominal examination
o Fundal height
o Foetal heart
o Foetal movement
o Foetal parts
o Presentation
o Twin pregnancy
b. Ultrasound
c. Other examinations (RH Immunoglobulin)
v. Mental Preparation
Sufficient time & opportunity should be given to expectant mother to have free & frank talk on all aspects of pregnancy & delivery.
Family Planning
Mother is psychologically more receptive to advice of family planning at this time. Educational & motivational efforts must be initiated during antenatal period for family planning.
c. Natal Care
It means care of mother & child during child birth. Child birth is a normal physiological process but complications may arise. Therefore need for intra natal care is necessary.
Emphasis is made on cleanliness. It means:-
o Clean hands & fingers
o A clean surface for delivery
o Clean cutting & care of the cord
o Keeping Birth Canal Clean by avoiding harmful practices.
o Clean gloves, towel, etc.
Aims of Natal Care
o Thorough Asepsis
o Delivery with minimum injury to the infant & mother
o Readiness to deal with complications such as prolonged labour, antepartum hemorrhage, convulsions, malpresentation, prolapse of cord etc
o Care of the baby at delivery- resuscitation, care of the cord, care of the eyes.
o Delivery by trained personnel
o Detect & treat appropriately infectious diseases of birth canal
o Effective transportation to a referral facility
d. Post-natal Care
Care of the mother & the newborn after delivery is known as post-natal or postpartum care.
Objectives of Postnatal Care
o To prevent complications of the postpartal period
o To provide care for the rapid restoration of the mother to optimum health
o To check adequacy of breast feeding
o To provide family planning services
o To provide basic health education to mother/family
o Immunization of the child
o Nutritional guidance for the mothers
o Exercise
o Psychological assistance
o Preventing Maternal Deaths
The 5 steps that a physician can take to prevent the large majority of maternal deaths:
1. Provide good antenatal care.
2. Conduct/supervise delivery in clean safe environment by a trained birth attendant.
3. Prevent prolonged labor; refer early any delay in labor (in primigravida beyond 12 hours, and in multiparae delay beyond 8 hours) for appropriate management.
4. Provide emergency care promptly to women with postpartum bleeding and refer them early to hospital, (good referral system)
5. Counsel couples on adopting contraception to avoid unnecessary pregnancies through contraception rather than taking recourse to unsafe abortion.
 howMed Know Yourself
howMed Know Yourself