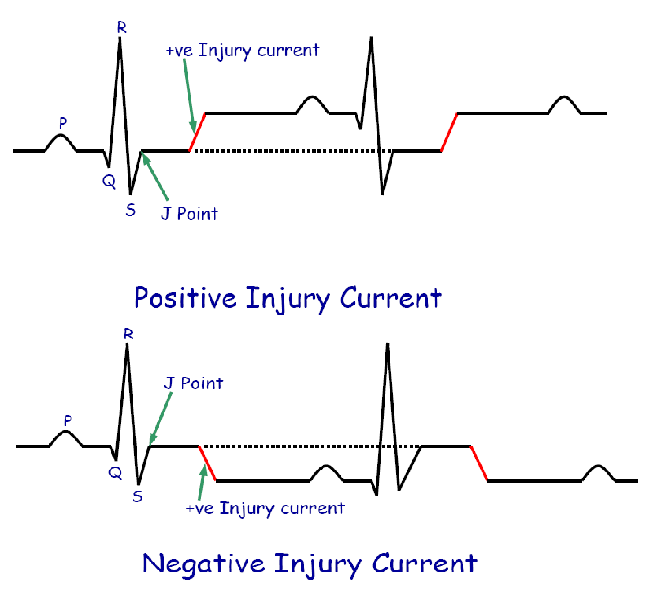
Flow of current from damaged area to normal area of heart between heart beats is called current of injury
Damaged area (semi-viable)
Remains depolarized (negative outwards)
Vector of injury current points towards normal part of heart (positive)
Base of vector lies in damaged area of the heart (negative)
Causes
Ischemia (most common cause)
O2lack, Co2accumulation, nutrients deficiency →depression of Na+/ K+Pump
Mechanical trauma
Ruptures the cell membranes
Infections
Ruptures the cell membranes
Damaged myocardium (permanently -ve) will affect the pattern of repolarization
Injury current represents the mean recordable repolarization vector (incomplete ‘T wave’ vector)
Repolarization is not complete so ‘T wave’ will not come to base line
Injury current Positive or negative
Depends upon the relation between current of injury vector and +ve electrode of the respective lead
Injured myocardium
Produces injury currents →ST segment shift on ECG
Infarcted(dead) myocardium
does not generate electrical activity →SignificantQ waves on ECG
Normal myocardium suffering from mild ischemia
Repolarization starts early in ischemic area →T wave vector shifts → change in T wave morphology
Arrhythmia
Irregular heart beat
Normal Sinus Rhythm (NSR)
Rhythm generated by SA nodeat a rate of 60 to 100beats per minute with sequential inscriptionof P–QRS–T waves at regular intervals
Sinus Tachycardia
Normal sinus rhythm with heart rate more than 100 beats per minute
Causes
Exercise, emotions, fever, hyperthyroidism etc
ECG finding
Decreased RR interval < 0.6 seconds (< 3 large squares)
Sinus Bradycardia
Normal sinus rhythm with heart rate less than 60 beats per minute
Causes
Sleep, Athletes, drugs (beta blockers) etc
ECG findings
Increased RR interval > 1.0 seconds (> 5 large squares)
Sinus Arrhythmia
Fluctuation in heart rate with phases of respiration
Increase during inspiration
Decrease during expiration
A normal phenomenon
Mediated by parasympathetic system
Decreased sinus arrhythmia may lead to rhythm problems
Cause
Inhibition of cardioinhibitory area
Stimulation of stretch receptors in lungs
Afferents through vagal nerve to cardioinhibitory area
Spillover of signals from respiratory center to vasomotor center
ECG findings
Variable RR intervals (heart rate variability)
Heart Blocks
Blockage of impulse conduction
Intra-atrialblocks
Atrioventricular blocks
Intraventricular blocks
Intra-atrialblocks
Sinus arrest (sick sinus syndrome)
SA node fails to generate an impulse
Sino-atrialblock
Impulse is generated but it is blocked to enter the atria
A complete cycle (P-QRS-T) is missed
SA node resumes pacing or any other potential pacemaker takes over
Incomplete heart blocks
First degree heart block
PR interval more than 0.2 seconds
Second degree heart block
Gradual lengthening of PR interval until blocking the impulse –Wenckebachphenomenon
Intermittent conduction of impulse from atria to ventricles –Mobitz phenomenon
P : QRS = 2 : 1 or 3 : 2 or 3 : 1 etc
Complete heart block
Third degree heart block
Total blockade of impulse conduction from atria to ventricles
Atrioventricular dissociation
Ventricles escape
Idioventricular rhythm
Atria pace at their own rhythm
Stokes-Adams syndrome
Intermittent complete AV block
Due to border line ischemia of conductive system
Fainting due to lack of blood supple to brain
Ventricular escape after about 5-30 seconds due to overdrive suppression
Right bundle branch block
Left bundle branch block
Electrical alternans
Conduction block in terminal purkijefibers
The pacemaker of heart
When SA node fails
Ectopic pacemakers take over
Present in conducting fibers
Atrial ectopic focus
Inherent rate -60 to 80 per minute
AV nodal (junctional) ectopic focus
Inherent rate -40 to 60 per minute
Ventricular ectopic focus
Inherent rate -15 to 40 per minute
Escape beat
Response of ectopic pacemakers to pause in cardiac electrical activity from SA node
Escape beats
Atrial escape beat
Nodal (junctional) escape beat
Ventricular escape beat
Escape rhythm
Atrial escape rhythm
Atrial ectopic focus (60-80 beats/min)
Nodal (junctional) escape rhythm
Junctional ectopic focus (40-60 beats/min)
Ventricular escape rhythm
Ventricular ectopic focus (15-40 beats/min)
Pathologic & irritable pacemakers
Ectopic pacemakers present in conducting system
Ectopic pacemakers in cardiac muscle cells
Pathologic and irritable pacemakers lead to arrhythmias with heart rates over 150 per minute
Premature contractions
A contraction that appears before its expected time from an irritableectopic focus
Also called extrasystole or premature beat
Premature atrial contraction
Premature nodal or junctional contraction
Premature ventricle contraction (PVC)
Irritable ectopic foci
Occasional discharge leads to Premature contractions
Repetitive discharge leads to Paroxysmal tachycardias, flutter or fibrillation
Paroxysmal tachycardia
Heart rate from 150 to 250 per minute
Sudden attack of tachycardia
Tachycardia abolishes by itself
Cause
Pacing from irritable ectopic foci
Re-entry mechanism
Paroxysmal tachycardia
Atrial
Nodal
Ventricular tachycardia -run of PVCs
Flutter
Heart rate from 250 to 350 per minute
Cause
re-entry (circus movement)
Multiple irritable ectopic foci
Fibrillation
Hear rate from 350 to 450 per minute
Cause
re-entry (circus movement)
Multiple irritable ectopic foci
Flutter & Fibrillation
Flutter
Atrial
ventricular
Fibrillation
Atrial
Ventricular
Ventricular fibrillation
A serious emergency
Many areas of ventricles contract simultaneously
Rate on ECG 350-450 per minute
Ventricles can’t pump blood
Leads to death if not treated
Cause
Electric shock
PVC (R on T phenomenon)
Treatment
Electroshock (cardioversion)
Ventricles are thrown into refractoriness
New impulse generates at SA node
Cardiopulmonary resuscitation (CPR)
Re-entry (Circus movements)
Propagation of cardiac impulse continuously within a closed circuit
Prerequisites for re-entry
Long pathway
dilated heart
Low velocity of conduction
Ischemia, conduction blockade, increased ECF K+
Shortened refractory period
Epinephrine, repetitive electric stimulation
Chain reaction mechanism
A mechanism to develop ventricular fibrillation
Simultaneous appearance of refractory and excitable areas
Division of impulses
Establishment of re-entry circuits
Vicious circle of impulse formation & patches of refractory areas
CLINICAL USE OF ECG
Heart rate
Rhythm
Infarction
Hypertrophy
Axis deviation
Electrolyte imbalance
Drug toxicity
 howMed Know Yourself
howMed Know Yourself