Neisseria meningitidis, a gram negative cocci, is one of the three important bacteria causing meningitis. People with deficiencies of late acting complement components have an increased incidence of meningococcal bacteria.
 Pathogenesis
Pathogenesis
Entry
- Transmission occurs by airborne droplets
- It colonizes the membranes of nasopharynx and upper respiratory tract
Spread
From the nasopharynx the organism enters into bloodstream and spreads to:
- Meninges
- Joints
- Disseminate throughout the body causing meningococcemia
Virulence Factors
- Polysaccharide capsule
- Endotoxin –lipopolysaccharide (LPS)
- IgA protease
a. Polysaccharide Capsule
Enables the organism to resist phagocytosis by polymorphonuclear leukocytes.
b. Lipopolysaccharide
Causes fever, shock, in purified form can reproduce many of the clinical manifestations of meningococcemia
c. IgA protease
Helps bacteria to attach to the membranes of upper respiratory tract by cleaving secretory IgA.
Predisposing Factors
- Late acting complement components (C6-C9) deficiencies
- Closed/crowded environment
- Malnutrition
- Poor hygiene
- Decreased neutrophils
Clinical Symptoms
- Asymptomatic carriage
- Acute meningitis
- Meningococcemia
- Waterhouse Friderichsen syndrome
Symptoms of Meningitis
- Severe headache
- Stiff neck
- Dislike of bright light
- Fever
- Vomiting
- Rash
- Drowsiness
Laboratory Diagnosis
Specimen
- CSF
- Blood
- Swabs from hemorrhagic skin lesions
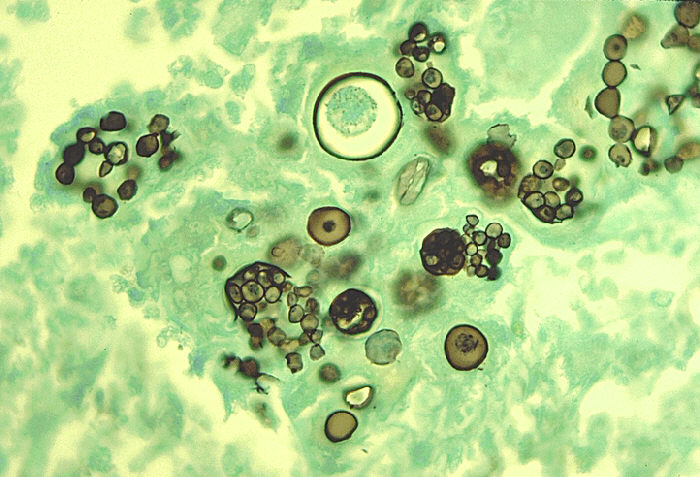
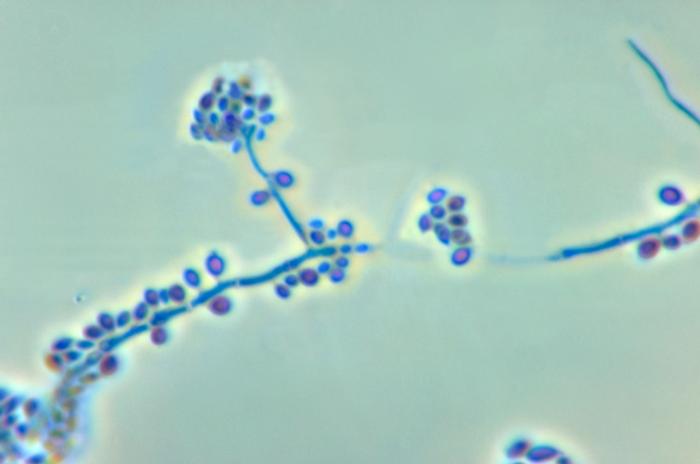
Microscopy
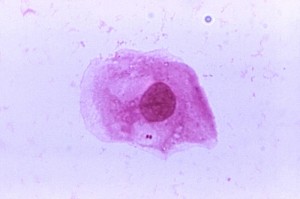
Microscopy reveals:
- Gram negative diplococcic
- Kidney shaped
- Non-motile
- Non-spore forming
- Fastidious organisms
- With Leishman stain, polymorphonuclear neutrophils are seen
Examination of CSF
On examination of CSF, it is seen that there is:
- Decreased glucose
- Increased lymphocytes
- Increased proteins
- Color is yellow
Culture
On chocolate agar, grey shiny colonies are observed, on incubation at 37ºC in 5% C02
Mueller Hinton agar may be used as well.
Biological Tests
- Catalase positive
- Oxidase positive
- Ferments glucose
- Ferments maltose
- DNAase negative
- Β-galactosidase negative
- Glutamyl-aminopeptidase positive
Serological Tests
- Latex agglutination test positive
- Serum antibodies are not useful
- PCR may be performed
Treatment
- Benzyl penicillin
- Chemoprophylaxis
- Vaccination
Want a clearer concept, also see
Lecture on Neisseria Meningitidis
things to write an essay about
 howMed Know Yourself
howMed Know Yourself