Gout is a group of metabolic diseases associated with hyperuricaemia and deposition of crystals of monosodium urate in tissues. Presentation usually occurs in males over 30 years of age and in females after the menopause.
Stages
1. Asymptomatic hyperuricaemia
The hyperuricaemia is usually present for many years before the onset of symptoms. It is important to point out that only one in 20 subjects with hyperuricaemia will go on to develop clinical gout.
2. Acute gouty arthritis
The classical presentation is acute inflammation of the metatarsophalangeal joint of the big toe (70%). The first attack is usually monarticular-other joints that may be involved are the ankle, knee, wrist, elbow, small joints of hands and feet.
3. Recurrent / Intercritical gout
Some patients may only have one attack whilst others have recurrent attacks at shorter and shorter intervals. Between attacks the patient is usually normal except for hyperuricaemia.
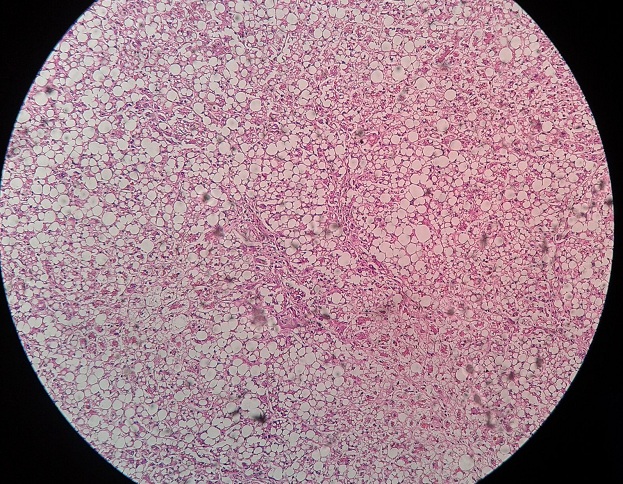
4. Chronic tophaceous gout
This follows recurrent acute attacks and is characterized by the development of tophi (swellings containing uric acid crystals) in the periarticular tissue. Other sites include the helix of the car, bursae and tendons.
Complications
Urolithiasis
Ten per cent of gouty patients develop urate stones and 10% of all renal calculi are due to urate.
Renal failure
Acute renal failure due to acute obstructive uropathy (urate crystals) may occur during cytotoxic therapy for malignancy (allopurinol cover should be used); it has also been described in gouty subjects after severe exercise. Progressive chronic renal insufficiency is an important cause of morbidity and mortality in untreated chronic tophaceous gout.
Associated Conditions
Gout and hyperuricaemia are often associated with
● Obesity,
● Alcoholism,
● Hyperlipidaemia,
● Impaired glucose tolerance
● Ischaemic heart disease
Diagnosis
It is important to recognize that:
● Hyperuricaemia is not synonymous with gout (1 in 20 develop gout)
● An acute gout attack may be associated with a normal plasma urate level although hyperuricaemia will be demonstrated at some stage.
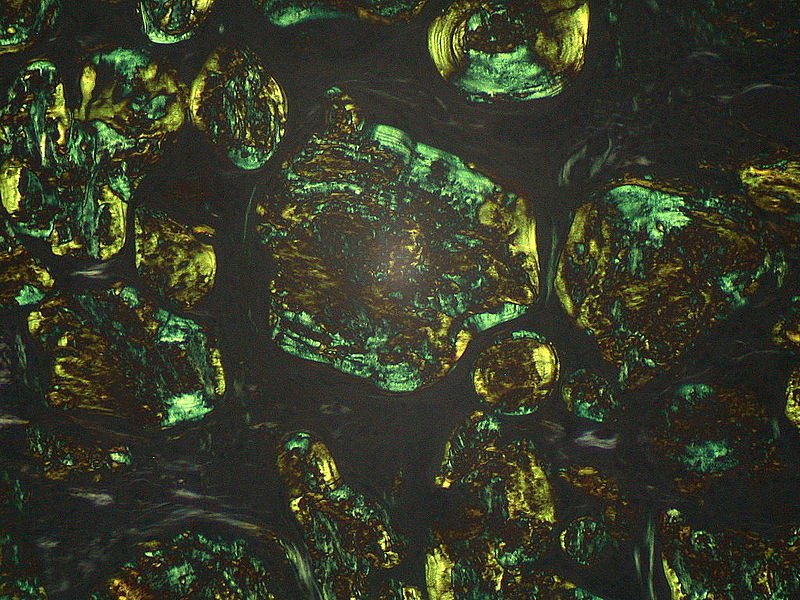
● Whenever possible, synovial fluid should be obtained and examined under polarizing light microscopy for monosodium urate crystals. Urate crystals are needle-shaped and strongly negatively birefringent. Pyrophosphate crystals (cause of pseudogout) are weakly positively birefringent and rhomboidal in shape.
Laboratory Investigations
Useful estimation in the evaluation of hyperuricaemia and gout are plasma urate, plasma Creatinine (renal function) and urinary urate.
1. Plasma urate
The plasma urate is influenced by a wide variety of factors
Race: For example, markedly raised in Maoris
Sex : Higher in males
Age : Higher is older age groups
Body mass: Elevated in obesity
Exercise: Increase (lactate effect)
Pregnancy:Levels initially fall by up to 25% in the first trimester, but then rise to values 20% higher than in the non-pregnant state; this elevation is maintained for a month or two.
Elevated levels:
- High meat (purine) intake
- Alcohol ingestion
- Lactate decreases renal excretion
- Alcohol increases ATP turnover
- Purines in beer yeasts
- Fasting (ketones inhibit renal urate excretion and there is increased purine degradation)
2. Plasma Creatinine :
Hyperuricaemia may cause renal failure and renal failure will result in hyperuricaemia. As renal failure progresses the plasma urate rises to a level of around 0.6 mmol/L and then plateaus; thus, a urate in excess of 0.6 mmol/L suggests that renal failure is not the only cause of the high urate.
3. Urinary Urate
Hyperuricaemia may be due to overproduction or decreased renal excretion or both. The rate of renal urate excretion provides a rough index of the production rate, providing renal function is normal.
Therapeutic agents used in gout and hyperuricaemia
Three groups of drugs are available for the management of gout and hyperuricaemia:
- Allopurinol
- Uricosuric agents
- Anti-inflammatory agents
For more detail, see drug treatment of gout
 howMed Know Yourself
howMed Know Yourself