Intracellular accumulations include the following:
1. Water (hydropic change)
2. Fatty change: fats may accumulate in the liver as fatty change
3. Cholesterol & esters: sphingolipidoses and other lipid accumulations
4. Proteins: abnormal protein accumulation is often irreversible.
5. Glycogen: glycogen storage diseases
6. Complex carbohydrates: mucopolysaccharidoses and other complex carbohydrate diseases.
7. Minerals: iron, as hemosiderin, or carbon, as anthracotic pigment
8. Pigments
9. Calcium
10. Amyloid
Causes
Intracellular accumulations may take place by:
1. Increased production of normal products due to inadequate functioning
2. Defective mechanism of removal of normal/abnormal substance which has accumulated
3. Increased exogenous substance with no removal mechanism.
Fatty Change
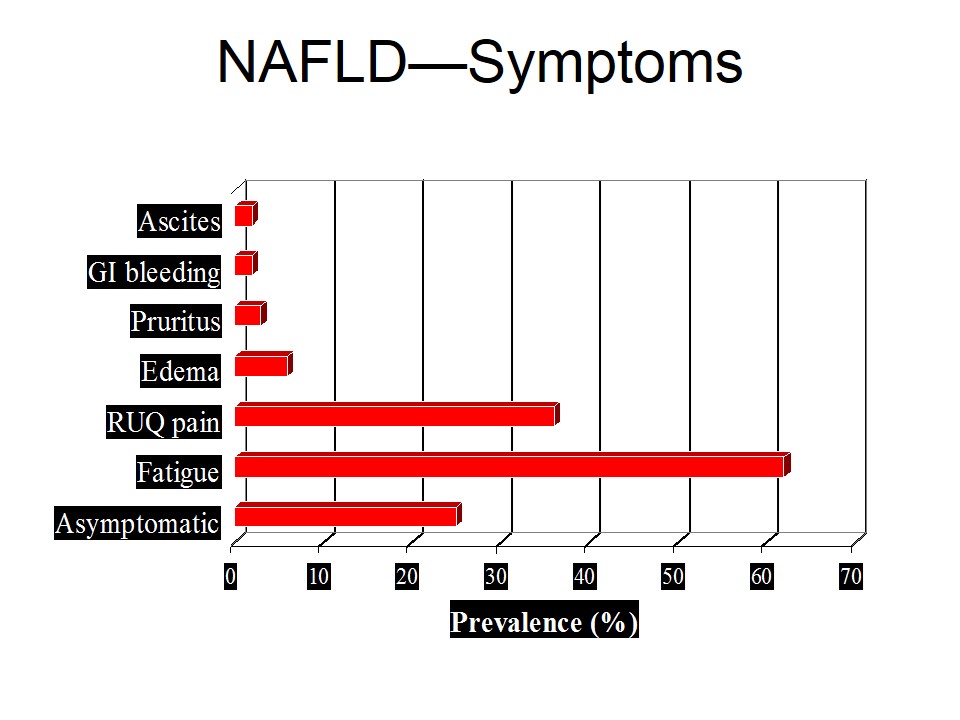
Accumulation of excessive lipid in cells is known as fatty change. It may occur in liver, heart or the kidneys.
Hepatic lipid accumulation is characterized by intracellular accumulation of triglycerides, and due to the failure of metabolic removal. Defects in fat metabolism are often induced by alcohol consumption, and also associated with diabetes, obesity, and toxins. Fatty change is most often seen in the liver (and heart), and is generally reversible.
Fatty acids enter hepatocytes, triglycerides combine with apoproteins and exit the liver. Defect in any of these above steps may lead to fatty change.
Causes of Fatty Change
Causes of fatty change include:
1. Toxins, alcohol
2. Protein malnutrition
3. Diabetes mellitus
4. Hypoxia ,anemia, ischemia
5. Drugs, pregnancy & obesity
Morphology of Fatty change
Gross morphology in liver depends on severity. Increased size is observed and liver becomes yellow and greasy when severe.
Histology
Microvesicular cytoplasm or macrovsicular cytoplasm is seen.
Microscopy
Fat vacuoles coalesce and displace the nucleus to the periphery of the cell. Vacuoles appear clear, with well-defined edges. Lipid accumulations must be distinguished from accumulations of water or glycogen, using special preparation and stain – Oil Red-O.
Cholesterol and Esters
Cholesterol & esters accumulate in macrophages (foam cells) and foreign body giant cells, resulting in:
a. Atherosclerosis
b. Hereditary & aquired hyperlipidemias with xanthoma formation
Pigments
Pigments may be endogenous or exogenous:
1. Endogenous
– Hb derived iron, bilirubin
– Non Hb derived melanin, lipofusion
– Melanin -Brown pigment synthesized in melanocytes which protects nuclei of basal epidermal cells from UV light.
– Malignant melanoma of eye, rectum
2. Exogenous
– Anthracosis -Accumulation of carbon, black pigment
– Tatooing
Bile pigment (bilirubin)
Bilirubin is derived from heme of Hb from destroyed RBCs in reticuloendothelial system. It is conjugated in hepatocytes with glucuronic acid & excreted as bile. Increased bilirubin may occur due to:
a. Hyperbilirubinemia, jaundice
b. Hemolysis, liver disease, obstruction to outflow of bile.
Excess iron accumulation
Total body iron is 2-4 gms. In functional pool, it is present in Hb, myoglobin, cytochrome and catalase. In the storage pool, it is present in macrophages of reticuloendothelial cells as Fe3+, ferritin or hemosiderin. It gives Purssian blue reaction.
Iron overload
Iron overload may occur due to:
• Localized increase in iron in tissue
a. Hematoma
b. Chronic venous congestion lung, heart
• Systemic increase in iron
a. Hemosiderosis, Fe in RES without damage
b. Hemolytic disease
c. Multiple blood transfusions
d. I/V Fe administration
Idiopathic hemochromatosis
Lack of regulation of iron absorbtion & defects in monocyte macrophage system leads to hemochromatosis. Iron gets deposited in liver, pancrease & RES, resulting in fibrosis, secondary diabetes mellitus, liver cirrhosis & cancer.
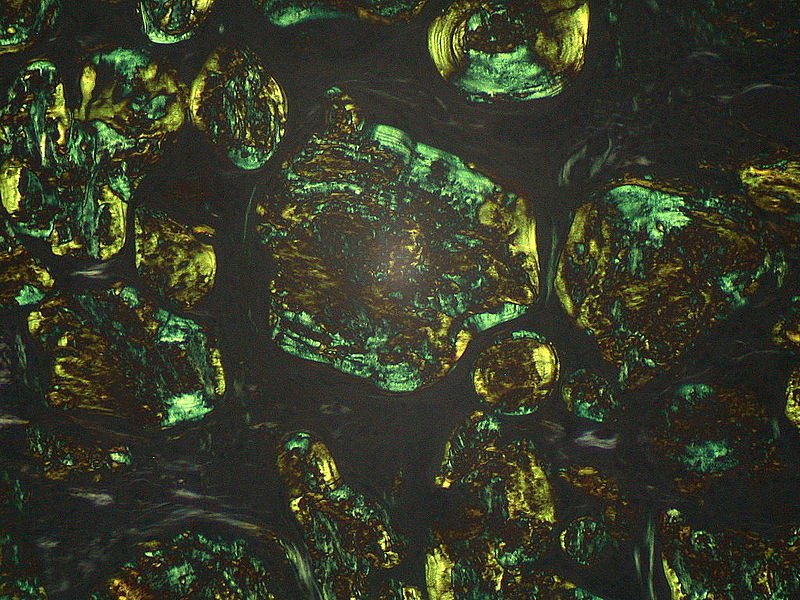
Haemosiderin
Haemosiderin is derived from hemoglobin. It is a golden yellow, granular or crystalline pigment and is the storage form of iron. It forms in response to local or systemic excess of iron. Ferritin forms hemosiderin granules.
• local excess: from gross or minute hemorrhage (eg. bruise)
• systemic excess: from increased absorption of dietary iron, impaired use of iron, hemolytic anemia, transfusions
Lipofuscin
Lipofuscin is the brown pigment in cytoplasm, which is oxidized lipid, derived from digested membrane organelles. It is part of aging process and atrophy in which lipid peroxidation occurs. It is harmless to cells and increased amount is seen in brown atrophic organs.
It is also known as “wear & tear” pigment derived through lipid peroxidation of polyunsaturated lipids of subcellular membranes. It accumulates in tissues undergoing slow, regressive changes – common in liver and heart of aging patients or patients with severe malnutrition and cancer cachexia.
It appears as a yellow-brown, finely granular, intracytoplasmic (or perinuclear) pigment.
Nevi
There are many, many adjectives and classifications of nevi. The MAIN things to differentiate these from melanomas. They may be:
• Junctional (more pigmented, more closely associated with melanoma)
• Intradermal
• Compound (both)
Malignant Melanoma
Malignant melanomas are malignant proliferations of melanocytes. The incidence of malignant melanoma is rising. It is related to sun like all skin cancers. It is the only primary skin cancer that can kill (except for the rare Merkel cell tumor). It quickly metastasizes, having both vertical and horizontal growth phase.
It is difficult to differentiate from nevus clinically and often microscopically.
Pathogical Calcification
Pathological calcification is of two types:
1. Dystrophic calcification
Abnormal CaPO4 in dead or dying tissue. Examples include:
a. Arterial wall as
• medial calcific sclerosis.
• Atherosclerosis &
• valvular heart disease.
b. In areas of tissue necrosis
• caseation ,
• coaggulative or
• fat necrosis
c. Dead parasite & their ova.
2. Metastatic calcification
Calcium deposition in normal tissue due to hypercalcemia. Examples include:
– Increased PTH leading to bone resorption.
– Metastatic bone tumor leading to bone resorption.
– Chronic renal failure
– Increased vitamin D
Common sites are kidney, stomach, lungs
Morphology
With H&E stain : basophilic amorphous granular appearance
Von Kossa stain – black deposits
For a clear concept, also see
 howMed Know Yourself
howMed Know Yourself