Nephrotic syndrome is characterized by excessive glomerular permeability to plasma proteins (proteinuria more than 3.5 g per day).
- Depending on the lesions, the proteinuria can be highly selective, for example, primarily low molecular-weight proteins (chiefly albumin).
- With more severe injury, nonselective proteinuria includes higher-molecular-weight proteins in addition to albumin.
- Heavy proteinuria leads to hypoalbuminemia, decreased colloid osmotic pressure and systemic edema.
- There are also sodium and water retention, hyperlipidemia, lipiduria, vulnerability to infection and thrombotic complications (the last resulting from loss of serum anticoagulants and antiplasmins).
Causes of Nephrotic Syndrome
Primary Glomerular Disease
- Membranous glomerulopathy
- Minimal change disease
- Focal segmental glomerulosclerosis
- Membranoproliferative glomerulonephritides
- Other proliferative glomerulonephritides (focal, pure mesangial, IgA nephropathy)
Systemic Disease
- Diabetes mellitus
- Amyloidosis
- Systemic lupus erythematosus
- Drugs (non-steroidal anti-inflammatory, penicillamine, street heroin)
- Infections (malaria, syphilis, hepatitis B and C, acquired immunodeficiency syndrome)
- Malignant disease (carcinoma, sarcoma)
- Miscellaneous (bee-sting allergy, hereditary nephritis)
Systemic diseases with nephrotic syndrome
Diabetic glomerulopathy
- Nodular glomerulosclerosis (Kimmelstiel-Wilson disease)
Epidemiology
i. Glomerulopathy occurs in type 1 and 2 diabetes. Occurs more often in type 1 (35-45%) than type 2 diabetes (20%)
ii. Most common cause of chronic renal failure in United States.
| Glomerular disease | Clinicopathologic findings |
| Minimal change disese (lipoid nephrosis) |
Secondary causes: Hodgkin’s lymphoma
|
| Focal segmental glomerulosclerosis |
|
| Diffuse membranous glomerulopathy | Second most common cause of nephrotic syndrome in adults are primary and secondary types;
secondary causes:
|
| Type I MPGN |
|
| Type II MPGN |
|
CRF, chronic renal failure; EM, electron microscopy: CBM, glomerular basement membrane; HBV, hepatitis B; HCV, hepalitis C; ICs, immun-complexes; IF, immunofluorescence; MPGN; membranoproliferative glomerulonephritis; SLE, syslemic lupus erylhematosus; VECs, visceral epithelial cells.
Risk factors
(a) Poor glycemic control
(b) Hypertension
(c) Diabetic retinopathy
High correlation with coexisting glomerulopathy
Pathogenesis
Nonenzymatic glycosylation (NEG) of the glomerular basement membrane
Also affects tubule basement membranes
i. Glycosylation refers to glucose attaching to amino acids
ii. Increases vessel and tubular cell permeability to proteins
NEG of the afferent and efferent arterioles
a. Produces hyaline arteriolosclerosis
b. Involves efferent arterioles before afferent arterioles
Osmotic damage to glomerular capillary endothelial cells
a. Glucose is convereted by aldose reductase into sorbitol
b. Sorbitol is osmotically active
c. Water enters the cells causing damage.
Hyperfiltration damage to the mesangium
a. Selective hyaline arteriolosclerosis of efferent arterioles
b. Increases the GFR, which damage mesangial cells
Diabetic microangiopathy; increased deposition of type IV collagen
a. GBM, tubular cells basement membranes, mesangium
b. Nonspecific immunofluorescence
c. Electron microscope shows fusion of podocytes
Essentials of diagnosis
- May be primary or secondary to systemic infections (e.g secondary syphilis, endocarditis), diabetes, multiple myeloma with or without amyloidosis, heavy metals and autoimmune diseases.
- Anorexia dyspnea, anasarca, foamy urine.
- Proteinuria (>3 g/d), hypoalbuminemia (<3 g/d), edema, hyperlipidemia in 50% upon presentation
- Hypercoagulability with peripheral renal vein thrombosis, particularly in membranous nephropathy
- Lipiduria with oval fat bodies, Maltese crosses, and fatty and waxy casts in urinary sediment
- Further tests may include complement levels (CH50, C3, C4),
- Serum and urine electrophoresis, antinuclear antibody (ANA),
- Serologies (hepatitis B and C, syphilis),
- Renal ultrasound
- Renal biopsy if treatment implications present.
Differential Diagnosis / Causes
- Congestive heart failure; cirrhosis; constrictive percarditis
- Minimal change disease; amyloidosis
- Focal segmental glomerulosclerosis
- Diabetic nephropathy; membranous nephropathy
- Membranoproliferative glomerulonephritis
Mechanism:
Glomerular injury is due to cytokines not neutrophils.
- Cytokines damage podocytes causing them to fuse together
- Cytokines destroy the negative charge of the GBM
Clinical and Laboratory Findings
1. Key finding is proteinuria > 3.5 g/24 hours
2. Generalized pitting edema and ascites
a. Due to hypoalbuminemia
Pitting edema in nephritic syndrome is due to sodium retention
b. Increased risk for developing spontaneous peritonitis
Due to streptococcus pneumoniae
3. Hypertension in some types
- Due to sodium retention
4. Hypercoagulable state due to loss of antithrombin III
- Potential for renal vein thrombosis
5. Hypercholesterolemia
- Hypoalbuminemia increases synthesis of colesterol (unknown mechanism)
6. Hypogammaglobulinemia
- Due to the loss of gamma globulins in the urine
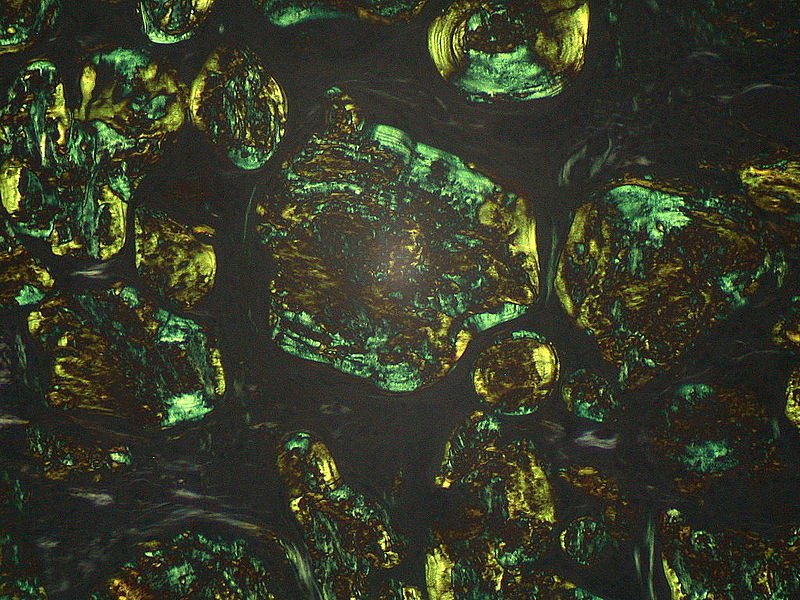
7. Fatty casts with maltese crosses and oval fat bodies
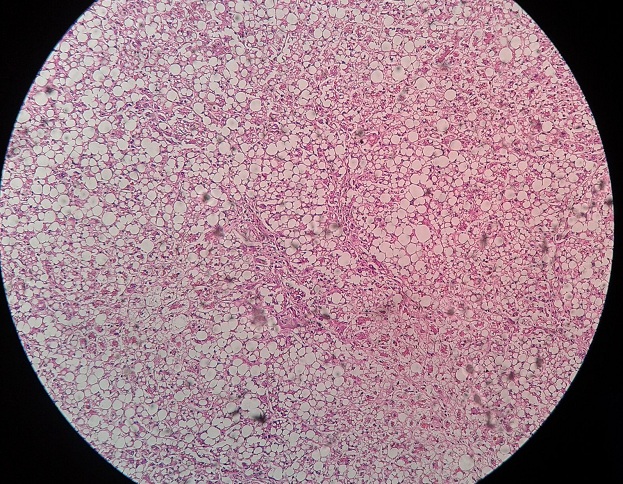
Microscopic Findings
1. Afferent and efferent hyaline arteriolosclerosis
When the afferent arteriole becomes hyalinized, the GFR decreases.
2. Nodular masses develop in the mesangial matrix
Due to increased type IV collagen synthesis and trapped proteins.
Treatment
- Supportive therapy with fluid and sodium restriction, diuretics to control edema, control of hypertension (with ACE inhibitor when possible), lipid-lowering agents, chronic anticoagulation for severe hypoalbuminemia or thrombotic events
- Maintenance of adequate nutrition.
- Corticosteroids for minimal change disease; idiopathic membranous nephropathy may be treated with corticosteroids and cytotoxic agents.
Pearl
- Given the therapeutic implications, renal biopsy should be seriously entertained in all patients with new onset of nephrotic syndrome.
 howMed Know Yourself
howMed Know Yourself