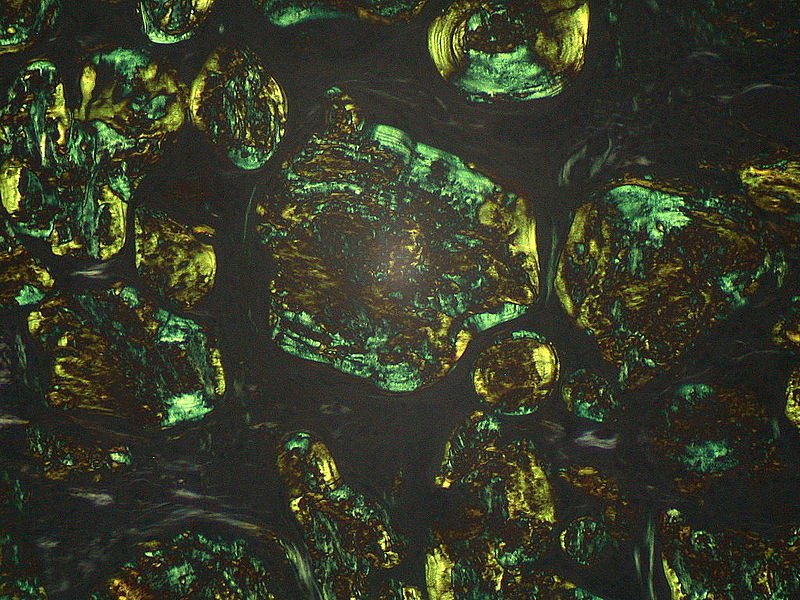
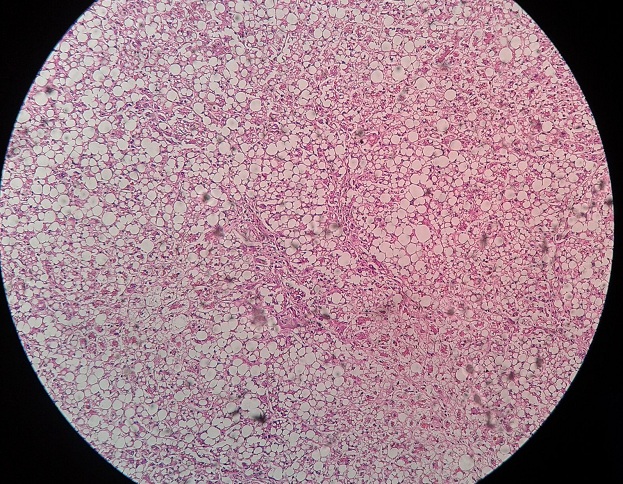
Nonalcoholic fatty liver disease is diagnosed from a liver biopsy showing moderate to gross macrovesicular fatty change with or without inflammation (lobular or portal), mallory bodies, fibrosis, or cirrhosis and with negligible alcohol consumption (less than 40 g of ethanol per week).
- History is obtained by three physicians independently.
- Random blood assays for ethanol should be negative.
- If performed, desialylated transferrin in serum should also be negative.
- Absence of serologic evidence of hepatitis B or hepatitis C.
Spectrum of Disease
a. Steatosis
b. Steatohepatitis (NASH)
c. NASH with Fibrosis
d. Cirrhosis
Prevalence and Importance
Prevalence of NAFLD is 13-18% and that of NASH specifically is 2-3% (1.2-9%). It is the leading cause of cryptogenic cirrhosis. It is a disease of all sexes, ethnicities, and age groups (peak 40-59). It occurs more frequently in females (65 to 83%).
Risk Factors
| Acquired Metabolic Disorders in 38% | *Obesity* |
| *Diabetes Mellitus* | |
| *Hypertriglyceridemia* | |
| Total Parenteral Nutrition ,Rapid weight loss, Acute starvation | |
| Surgery | Jejunoileal Bypass |
| Extensive Small Bowel Loss | |
| Medications | Corticosteroids; Estrogens |
| Amiodarone | |
| Methotrexate; Tamoxifen | |
| Diltiazem; Nifedipine | |
| Occupational ExposuresOthers | Organic SolventsWilson’s, Abetalipoproteinemia, Jejunal diverticulosis |
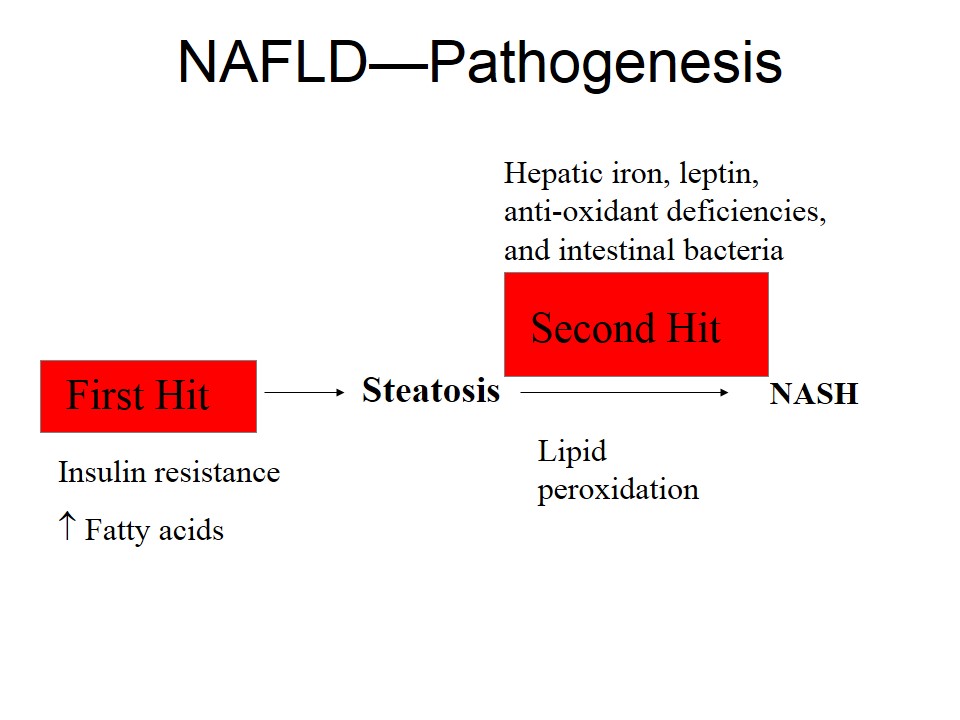
Pathogenesis
Triglyceride Accumulation
- The normal liver contains less than 5% lipids by weight
- There is excessive importation of free fatty acids in
- Obesity
- Rapid weight loss
- Excessive conversion of carbohydrates and proteins to triglycerides
- Impaired VLDL synthesis and secretion occurs in
- Abetalipoproteinemia,
- Protein malnutrition,
- Choline deficiency
- Impaired beta-oxidation of free fatty acids to ATP occurs in
- Vitamin B5 deficiency,
- Coenzyme A deficiency
Insulin Resistance
In insulin resistance, there is increased
- Peripheral lipolysis
- Triglyceride synthesis
- Hepatic uptake of fatty acids
In peripheral tissues, muscle and adipose, decreased uptake of glucose takes place. In liver, failure of insulin to stimulate glycogen synthesis and suppress gluconeogenesis leads to failure of insulin to downregulate hepatic glucose production.
Peripheral Insulin Resistance and failure of humoral mediator
- Resulting in steatosis and NASH
- Increased fatty acid uptake and synthesis (lipogenesis), suppression of mitochondrial B-oxidation, and impaired triglyceride secretion as VLDL.
- Alternatively, steatosis and NASH could be attributed to the combined effects of severe peripheral IR and relative failure of humoral (adipokine) mediators that combat the effects of high insulin levels and fasting hyperglycemia on hepatic lipid turnover.
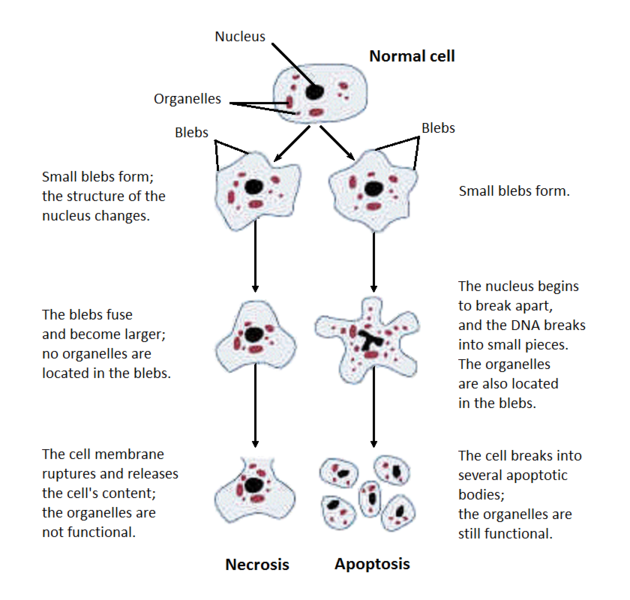
Lipid Peroxidation and Hepatic Lipotoxicity
Free radicals initiate the process derived from fat metabolism, in the setting of preexisting defects in mitochondrial oxidative phosphorylation. Free radical attack on unsaturated fatty acids. The products of the reaction are another free radical and a lipid hydroperoxide, forms a second free radical and, amplifies the process. Imbalance between pro- and antioxidant substances (oxidative stress) takes place.
Cytokine Activation and Fibrosis
Lipoperoxide induce expression of inflammatory cytokines. Cytokine level elevation, especially TNF-α has been well described in NAFLD.
Adiponectin and Leptin (Adipocytokines)
Adoponectin
A hormone secreted by adipose tissue. It enhances both lipid clearance from plasma and beta-oxidation of fatty acids in muscle. It has direct anti-inflammatory effects, suppressing TNF-alpha production in the liver
Leptin
Leptin is coded for by the obesity gene & governs satiety through action at the hypothalamus. Elevated levels in NASH were attributed to factors involved in production. No difference in leptin level was seen between patients with worsening injury or those without on serial biopsy. Resistance to leptin in the CNS rather than the liver may be important in the pathogenesis of NASH.
Abnormal Lipoprotein Metabolism
Natural History
Steatosis generally follows a benign course. It can progress to NASH ± fibrosis. NASH with fibrosis has increased liver-related morbidity and mortality. A study of 103 patients who underwent serial liver biopsies (mean interval between biopsies of 3.2 years) found:
– Fibrosis stage progressed in 37 percent
– Remained stable in 34 percent
– Regressed in 29 percent
Independent predictors of fibrosis progression
- Diabetes mellitus,
- Low initial fibrosis stage
- Higher body mass index.
- Elevated liver enzymes
Predictors of More Severe Histology in NASH
- Age >40–50 y
- Female gender
- Degree of obesity or steatosis
- Hypertension
- Diabetes or insulin resistance
- Hypertriglyceridemia
- Elevated ALT,AST, γ-GT level
- AST:ALT transaminase ratio >1
- Elevated immunoglobulin A level
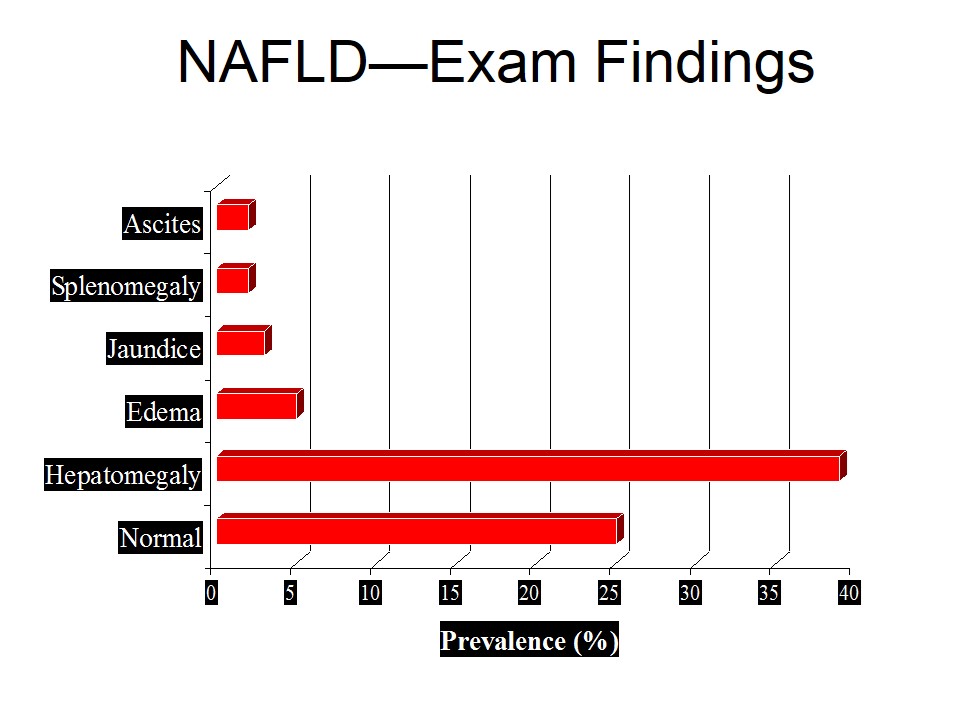
Laboratory Findings
- The AST/ALT ratio is usually less than 1 (90%)
- Antinuclear antibody positive in ~30%
- Increased IgA
- Abnormal iron indices in 20% to 60%
- Elevated PT and low albumin with cirrhosis
- Alkaline phosphatase is less frequently elevated
- Hyperbilirubinemia is uncommon
Normal labs do not rule out NAFLD
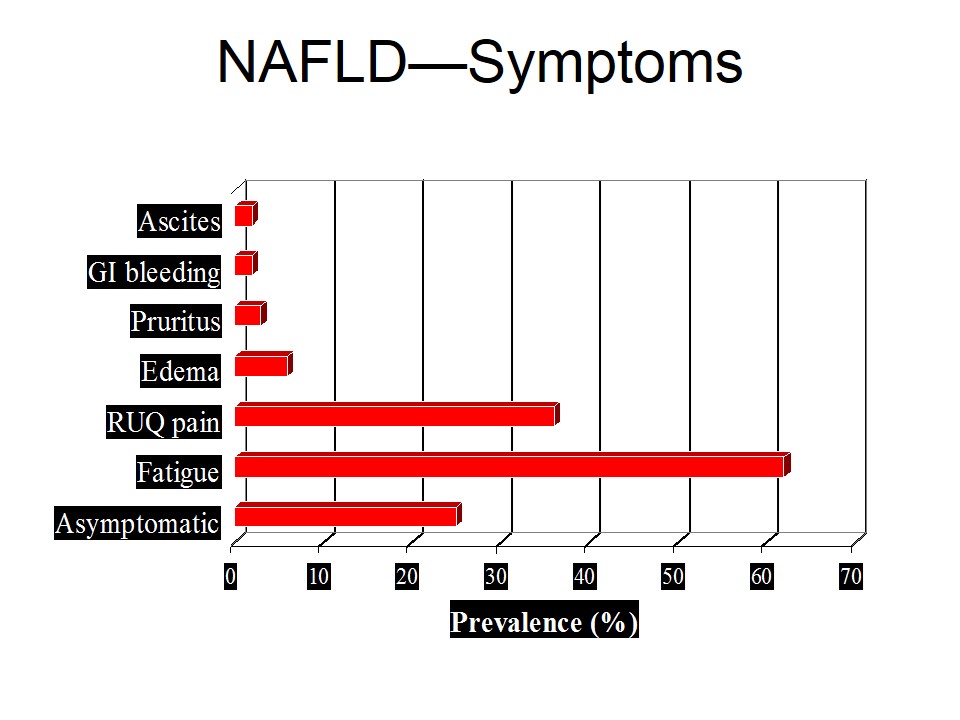
NAFLD—Imaging
Ultrasound
– Difficulty in differentiating fibrosis from fatty infiltration
– Misinterpretation of focal fatty sparing as a hypoechoic mass
– Poor detection if the degree of steatosis is less than 20% to 30%
– As initial testing in a suspected case and for large population screening, it is a reliable and economical
Computed Tomography
Sensitivity and specificity of detecting fatty liver (with spleen-minus-liver attenuation of 10 Hounsfield units) were 0.84 and 0.99
M R Spectroscopy
Correlation between liver fat concentration and 1H-spectroscopy was 0.9
Current non-invasive modalities are unable to detect NASH with or without fibrosis
Liver biopsy in NASH, Indications
- Peripheral stigmata of chronic liver disease
- Splenomegaly
- Cytopenia
- Abnormal iron studies
- Diabetes and/or significant obesity in an individual over the age of 45
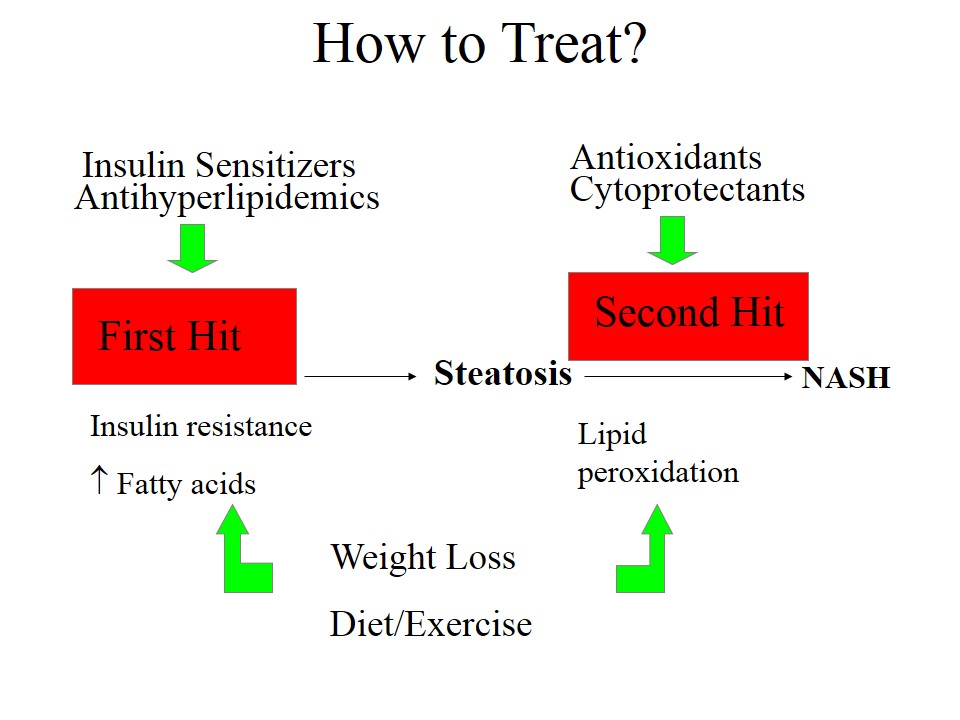
- There is no proven effective therapy for NASH.
- Gradual, sustained weight loss is hallmark therapy
- Attempts should be made to modify potential risk factors (obesity, hyperlipidemia, and poor diabetic control).
- Rapid weight loss potentially worsening of liver disease
- Gemfibrozil, & insulin sensitizers require further study
- Clofibrate, UDCA & Vitamin E are not useful in NASH.
 howMed Know Yourself
howMed Know Yourself