Clinical History
A-20 years old beautician, presented for evaluation of increased hair over her upper lip, chin, and sideburn area. Other areas also troubled her. The hair growth had become more noticeable over the last 7 years. Her menses began at age 12, occurred monthly for a year, then become progressively irregular in frequency and ceased entirely for the last year. She had no prior health problems and was taking no medications.
Family history:
Revealed that a paternal aunt had ‘a large amount of facial hair’.
On examination:
Female weight 145 Ib; height 63 inches; and BP 115/65. Terminal hair over the face, mid-anterior chest, linea alba and thighs was easily recognized. The skin was otherwise normal & had no striae, no temporal balding or hairline recession only a few acne scars. No breast discharge could be expressed. The external genitalia were normal. On bimanual pelvic exam, adnexal masses were palpable.
Questions:
1. What are the salient findings in history and clinical examination?
2. How do the clinical findings lead you to a provisional diagnosis?
3. Keeping in mind the above clinical findings what laboratory studies will you order to support the diagnosis in the case?
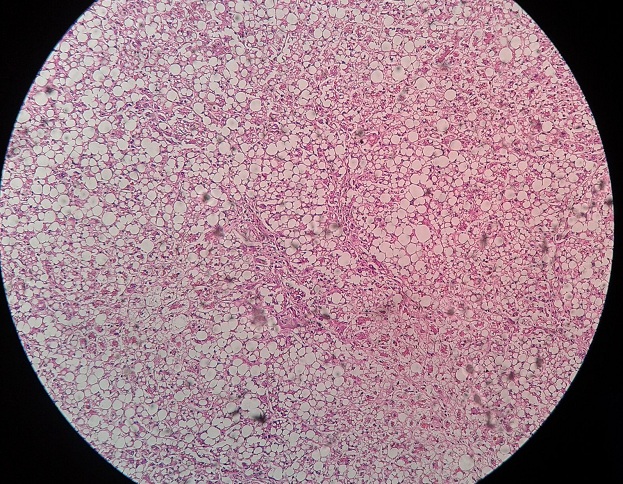
4. What are important factors of hirsutism and source of testosterone?
1. Polycystic ovary disease is the most likely diagnosis. Most women who present with hirsutism do not have any ominous cause but rather fit into a spectrum of syndromes associated with normal or modestly elevated serum testosterone and elevated free testosterone. These patients have varying degrees of ovarian stromal hyperplasia. Polycystic ovary disease (PCOS) is most common variant. It is characterized by chronic anovulation (amenorrhea/oligomenorreha), dysfunctional uterine bleeding) and slowly progressive hirsutism. A familial tendency may be noted for similar problems. Many patients are obese. Some women have no hirsutism but present for evaluation of infertility. Enlarged ovaries are palpable in about half of the subjects. The pelvic sonogram shows bilateral cystic ovaries in this patient (CLUE).
2. Laboratory studies: Need to evaluate this patient’s hirsutism include:
a. Serum testosterone
b. Free testosterone
c. Serum dehydro-3-epiandrosterone sulfate (DHEA-S)
d. Serum luteinizing hormone (LH) and follicle stimulating hormone (FSH)
e. Perform an overnight dexamethasone study.
f. In regard to amenorrhea, pregnancy should be excluded with a serum HCG.
g. When glactorrhea or amenorrhea is present, a serum prolactin is indicated.
Serum testosterone is usually elevated (>80 ng/dl but < 200 ng/dl), but if not the serum free testosterone will be elevated. Serum DHEA-S could be normal or minimally elevated. The ratio of LH to FSH is often elevated (LH/FSH > 2.5)
3. Hair growth in androgen-sensitive areas of the body results from the metabolism of androgens locally at the hair follicle
Increased circulating levels of free testosterone lead to binding of testosterone with androgen receptors at follicles of thin vellus. The testosterone receptor interaction stimulates 5-a-reductase, which converts testosterone to dihydrotestosterone (DHT), a very potent androgen responsible for proliferation and growth of thick terminal hair. Once 5-a-reductase is induced by testosterone other less potent androgens (such as DHEA and androstenedione) may serve as substrates for the enzyme leading to DHT formation. This system allows for a multiplier effect, in that weaker androgens now become stronger leading to local production of DHT within the hair follicle. The metabolism of testosterone at the hair follicle may be associated with a fall of serum testosterone levels despite continued hair growth.
Important Factors of Hirsuitism
• Include race (increased Caucasians)
• Genetic background (increased Mediterranean)
• Complexion (increased in blacks)
• Family history
Sources of Testosterone
1. Ovary 25% of the total
2. Adrenal 25% of the total
3. Peripheral tissues 50% of the total
 howMed Know Yourself
howMed Know Yourself