Some Patho-Physiological Aspects Of Diarrhea
Diarrhea means differently to different people.
Definition
Frequent and excessive loss of fluid and electrolytes accompanying:
- more than 200 grams of stool per day
- major portion is water à 70-80%
Fluid content and consistency grades
1. Grade I
Solid stool
2. Grade II
Semi solid stool
3. Grade III
Fluid and decal material mixed but its consistency is so much low that it takes shape of any container.
4. Grade IV
Water content and solid material separate.
5. Grade V
Only water content
For clinicians, grade IV and V are very dangerous, especially in children and elderly, because they rapidly develop dehydration and electrolyte imbalance.
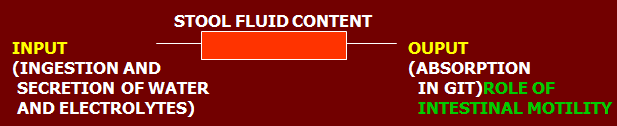
When absorptive capacity is exceeded or less time is provided for absorption, it leads to diarrhea
From Mechanistic prospective
It can be due to:
- Increased osmotic load in lumen
- Secretion of water and electrolytes in lumen
- Exudation of proteins and fluids from mucosa
- Increased intestinal motility
All these 4 mechanisms are readily affected by:
- Neurohormonal mechanisms
- Pathogens
- Drugs
Management
Correction Of Dehydration And Electrolyte Imbalance
- Oral rehydration therapy ORT – ORS
ORS basically exploits the nutrient dependent co-transport, which remains intact (Na and Cl transported always with glucose)
In condition where vomiting occurs, oral therapy is not effective:
I/V Rehydration
Normal saline (normotonic solution)
Ringer lactate (hypertonic solution)
So in patients, we start with Ringer’s lactate and then switch to normal saline. Never let the patient to die of hypovolemic shock.
Treat the cause
Symptomatic relief – drugs
Classification Of Anti-Diarrheal Drugs
1. Diphenoxylate
2. Diphenoxin
3. Loperamide
Adsorbents
1. Kaolin (attapulgite)
2. Pectin
Miscellaneous
1. Bismuth subsalicylte
2. Bismuth carbonate
3. Octreotide
4. Ispagullah husk and methylcellulose
Diphenoxylate
8-10 times more potent than morphine in decreasing gastrointestinal motility.
Mechanism of Action
Opioids in gut cause decrease in intestinal motility.
So, Diphenoxylate is converted into Diphenoxin/Diphenoxilic acid (active metabolite) producing anti diarrheal effect by three mechanisms:
- Inhibit presynaptic cholinergic nerve in submucosal and myenteric plexus by binding to peripheral mew receptors, that results in decreasing motility, leading to increased absorption of water.
- Increased tone of anal sphincter
- Increased mass colonic movements and gastrocolic reflex.
Side effects
Can cross BBB so adverse effects occur.
- CNS depression
- Respiratory depression
- Addictive potential
To counter addictive potential, it is marketed with small doses of atropine
Lomotil contains 2.5 mg diphenoxylate and 0.25 mg atropine.
Subtherapeutic doses do not have anticholinergic effect on this dose.
Motefen contains 1 mg diphenoxin and 0.025 mg atropine
Rationale of using atropine
So if patient will try to use more and more Lomitil, subtherapeutic doses of atropine are converted into therapeutic doses, producing anticholinergic effects leading to:
- Dryness of mouth
- Constipation
- Urinary retention
Loperamide
Mechanism of Action
Same mechanism of action, 40-50 times more potent than morphine in reducing gut motility.
Differences With Diphenoxylate
| Loperamide | Diphenoxylate | |
| Potency | More potent | Less potent |
| BBB | Does not cross | Crosses BBB |
| No CNS depression | CNS depression | |
| No addictive effect | Will occur, having analgesic effect in high doses | |
| Does not need atropine | Needs atropine |
Contraindications
- Ulcerative colitis
If given, increases chances of toxic mega colon (abnormal dilatation of colon) leading to increased risk of perforation and toxicity.
Ineffective diarrhea like:
- Acute bacillary dysentery –irritation of GI leading to diarrhea
- Amoebic dysentry
Anti motility drugs decrease the motility, leading to increased chances of toxin absorption, producing systemic adverse effects.
So as a rule, not used in children and infants.
Bismuth Subsalicylate
Mechanism of Action
Rapidly dissociates into bismuth and subsalicylate..
Bismuth then reacts with HCl and forms oxichloride which is not absorb at all.
- Anti-Bacterial Activity
Anti bacterial effect is by adsorbing bacteria. It binds bacteria and excretes them, very effective in H. pylori infections.
- Anti-Inflammatory Action
The other part of subsalicylate is rapidly absorbed and produces anti inflammatory effects by decreasing prostaglandins synthesis.
- Anti-secretory activity
Side Effects
Well tolerated drug.
- Black stools –darkening of stools, false impression of malena
- Dark coating of tongue
Methyl Cellulose & Ispagullah Husk
These two are not true anti diarrheals.
They absorb water and reduce fecal water content, leading to increased consistency of stools and giving false impression of bettering the diarrhea.
Orally proven uses of these are two:
- Colostomy
- Ileostomy
Kaolin And Pectin
Active form of Kaolin is Attapulgite – hydrated Mg Al disilicate
Pectin – indigestible carbohydrate derived from apple
Mechanism of Action
Both act as absorbants of bacterial toxins and fluids and decrease stool fluidity and frequency.
Side Effect And Caution
Well tolerated.
May cause constipation.
Used cautiously when other drugs are used because they will hamper their absorption.
Octreotide
Synthetic somatostatin analogue – peptide released in GIT & pancreatic d cells, enteric nerves and hypothalamus.
Mechanism of Action
- Inhibition of hormonal secretion
Decrease secretion of many hormones and neurotransmitters like gastrin, VIP and glucagon, insulin and CCK
- Decreases secretions
Decreases intestinal and pancreatic secretions
- Decreases motility
Inhibit contractions of gall bladder
- Decreases portal blood flow
By direct vasoconstrictor action
5. Decrease secretion of anterior pituitary hormones
Somatostatin half life is 2-3 minutes thus has limited clinical use
Octreotide half life is 1.5-2 hours, having the same actions
Uses
- Diarrhea due to vagotomy
- Short bowel syndrome
- AIDs
Octreotide has multiple effects on GI motility:
- High dose decreases motility (150-250 mcg/day)
- Low dose increases motility
- Carcinoid syndrome
- Tumors that secrete increased VIP
- Varices
Side effects
- GIT
a. Steatorrhea (absorption of fat soluble vitamins is decreased)
b. Abdominal pain
c. Flatulence
d. Diarrhea
On long term use:
- Acute cholecystitis
- Hyperglycemia or hypoglycemia because it alters balance between insulin, growth hormone and glucagon.
- Hypothyroidism
- Bradycardia
 howMed Know Yourself
howMed Know Yourself