In most of the cases, anti tussives are combined with mucolytics, mucokinetics and anti histamines (sedatives, anticholinergics are combined as well).
Cough
It is a protective reflex with sudden noisy expulsion of air , expelling sputum & other irritant materials from upper part of airways.
Types
(1) Productive / Useful Cough
It effectively expels secretions & exudates, from respiratory tract.
(2) Unproductive / Useless Cough
It is due to local irritation, e g smoker’s cough.
Anti-tussive Drugs:
Drugs which suppress cough & are used for symptomatic treatment of cough.
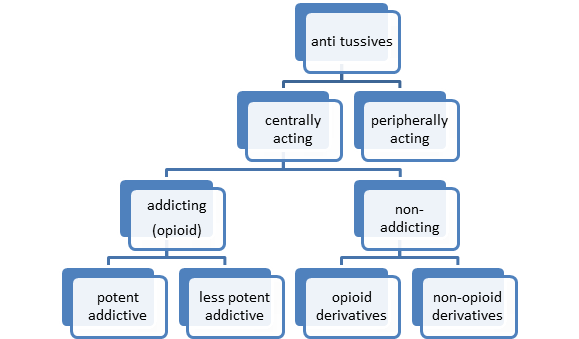
Types:
2 types according to mechanism of action
1. Centrally acting anti-tussives:
Suppress cough by a direct action on medullary cough center.
2. Peripheral Anti–tussives
They suppress cough reflex by decreasing the input of stimuli from cough receptors in respiratory passages.
Anti-tussive Drugs should be used to suppress unproductive / useless cough.
Classification of Anti-tussive Drugs
(A) Central Anti-tussives
(a) Opioid / Narcotic /Addicting Anti-tussives
(i) Less addicting Drugs
- Codeine phosphate,
- Pholcodine,
- Dihydrocodeine tartrate.
(ii) Potent addicting Drugs
- Morphine,
- Dihydromorphinone.
(b) Non-Addicting Anti-tussives
Opioid derivatives :
- Dextromethorphan,
- Noscapine.
Non Opioids:
- Benzonatate,
- Diphenhydramine –antihistamine 1st gen, having sedative, anticholinergic actions, crosses BBB
(2) Peripheral Anti-tussives
(a) Pharyngeal Demulcents (soothing action on irritating mucosa)
(b) Steam inhalation
With tincture bezoin / menthol.
(c) Drugs with Local Anesthetic Activity
- Benzonatate –has central and peripheral actions, local anesthetic so action on stretch receptors in lung bronchi
- Lignocaine by nebulizer –not anti tussive, only used in special cases (CA bronchus)
Uses
1) For dry unproductive cough.
2) If cough is unduly tiring.
3) Disturb sleep.
4) If patient is suffering from hernia, piles or underwent abdominal surgery
Mechanism of action of antitussives
Centrally acting
- Depression of medullary centres or associated higher centres.
- Increased threshold of cough centre.
Peripherally acting
- Interruption of tussle impulses from respiratory tract, having soothing effect.
Opioids:
Codeine
An opium alkaloid.
- It is more selective for cough centre.
- Centrally acting anti tussives increase threshold for cough.
- Suppresses cough for about 6 hours.
- The antitussive action is blocked by naloxone indicating that its action may be exerted through Opioid receptors in the brain.
- Cough suppression occur with low doses of opioids than those needed for analgesia.(sub-analgesic dose 15 mg)
- Abuse liability is low, but present.
Adverse Effects
- Constipation.
- Respiratory depression & drowsiness
- Driving may be impaired.
- Contraindicated in asthmatics & in patients with diminished respiratory reserve.
Pholcodeine:
- Centrally acting, suppresses center in medulla
- Little/ no analgesic or addicting property.
- Similar efficacy as antitussive to codeine
- Is longer acting—–acts for 12 hours or more.
- Given once or twice daily.
- Dose: 10-15 mg.
Adverse Effects
- Nausea
- Drowsiness.
Non-addicting Anti-tussives:
Noscapine:
- Depresses cough but has no narcotic, analgesic or dependence inducing properties.
- Efficacy same as codeine, specially useful in spasmodic cough.
Adverse Effects
- Headache & nausea can occur.
Dextromethorphan:
- A synthetic compound
- The d-isomer has selective antitussive action (raises threshold for cough & depresses cough center in medulla.).
- It has been found to enhance the analgesic action of morphine & other μ receptors agonists
- As effective as codeine, does not depress mucociliary function of the airway mucosa.
- Devoid of addicting actions.
- Produces less constipation than codeine.
- No CNS depression.
- Antitussive action for 6 hours.
- Naloxone does not antagonize it, indicating it does not act through opioids receptors.
- Available as combination with anti asthmatics drugs, bronchodilators, expectorants and anti histamines. Extended release preparation is available which is administered two times daily.
Side effects:
Dizziness, nausea, drowsiness & ataxia.
Dose: 15-30mg three or four times daily
Levopropoxyphene:
Devoid of opioid effect but has some sedative property.
Adverse Effects
Sedation.
Antitussive dose 50-100mg 4 hrly.
Antihistamines
- 1st generation drugs are used as anti tussives.
- Many antihistamines have been added to antitussive / expectorant formulations.
- They relieve cough due to their sedative and anticholinergic actions, but lack selectivity for the cough centre.
- Useful in allergic cough.
- They may reduce secretions by anticholinergic action (2-5 mg)
Diphenhydramine (15-25 mg) , Promethazine (15-25 mg) are commonly used.
Only first generation antihistamine are used, 2nd generation drugs cannot cross BBB, so having no sedative effect.
Peripheral Antitussives
Demulcents.
- They provide relief to throat.
- promotes salivation & inhibit impulses from inflamed mucosa.
Linctus
Thick liquid preparation containing sucrose and medicinal substance.
These have sedative, demulcent properties.
Throat lozenges:
- Small medicated tablets intended to dissolve slowly in mouth
- They have lubricating and soothing effect on irritated tissue of throat.
- Lonzenges may contain benzocaine or dextromethorphan.
Bronchodilators
- If cough is due to bronchospasm, D2 agonists are given.
- Bronchodilators relieve cough in patients with bronchial hyperreactivity.
- They shoud be used only when an element of bronchoconstriction is present.
Benzonatate:
Chemically related to Procaine, which is local anesthetic. It has both central and peripheral actions.
Mechanism of Action
- Exerts its antitussive action on stretch or cough receptor in lungs (Local anaesthetic effect).
- It has some central effects as well.
Adverse Effects:
- Headache,
- Dizziness,
- Pruritis
- Nasal Congestion,
- burning of eyes &
- tightness in chest.
Mucokinetics/Expectorants:
Definition:
Drugs which ↑ bronchial secretions or reduces its viscosity facilitating its removal by coughing
Expectorants
- Ipecacuanha
- Ammonium chloride
- Ammonium bicarbonate.
- Terepin hydrate
- Potassium Iodide
- Guaiphenesin
- Sodium or Potassium citrate.
Mechanism of Action of Mucokinetics
a. Directly acting:-
- Stimulate secretory cells of resp tract directly & produces demulcent effect by decreasing irritation and viscosity of mucous.
- Since these drugs stimulate secretion more fluid get produced in resp tract and sputum is diluted, there by helping in easy removal of sputum.
b. Indirectly/ reflex acting:-
- Act indirectly to relieve cough by irritating gastric mucosa and increases resp tract fluid secretion and decreasing viscosity of sputum.
Ammonium salts:
- Gastric irritants(nauseating) — enhance bronchial secretions.
- Expectorant doses are subemetic, having unpleasant taste.
- Used in combination with antitussives.
Ipecacuanha:
- Used as expectorant in small doses & emetic in large doses.
- It liquefies thick secretions and relieve the irritated mucosa.
- It also irritates the gastric mucosa and enhances the expulsion of secretion.
- It is mainly used for emesis in accidental poisoning.
Guaiphenesin
Mechanism of Action
Decrease sputum viscosity and increase sputum volume thereby decreasing difficulty in expectoration
Only FDA Approved expectorant .
Uses:
For symptomatic relief of dry, non productive cough in the presence of mucus in respiratory tract.
Adverse effects:
Gastric disturbances and drowsiness.
Mucolytics:
Drugs which render sputum less visous so that sputum is more easily cleared from chest.
Classification:
Inhalational:
- Acetylcysteine,
- Tyloxapol.
Oral :
- Acetylcysteine,
- Bromohexine,
- Carbocysteine,
- Methylcysteine.
Mechanism of Action
Acetyl – , Carbo – , & Methyl-cysteine
Split disulphide bonds in mucoprotein present in sputum & reduces its viscosity.
Bromohexine
Reduces viscosity of bronchial secretions by de-polymerization of muco-polysaccharides as well as liberating lysosomal enzymes , network of fibers in tanacious sputum is broken.
Clinical Uses
(1) Acute & chronic bronchitis.
(2) Bronchial asthma
Adverse effects
(1) CNS: Headache, tinnitus.
(2) GIT: GI disturbances, gastric irritation.
(3) Skin: Urticaria
Rhinorrhoea
Lacrimation.
Specific treatment approaches to cough
| Etiology of cough | Treatment approach |
| Upper/lower respiratory tract infection | Appropriate antibiotics |
| Smoking/ chronic bronchitis | Quit smoking / avoid Allergens/use antibiotic. |
| Pulmonary tuberculosis | Antitubercular drugs |
| Asthmatic cough | Inhaled β2 agonists/ ipratropium / corticosteroids |
| Postnasal drip due to sinusitis | Antibiotic, nasal decongestant, H1 antihistaminic |
| Postnasal drip due to allergic / perennial rhinitis | Avoid the precipitating factor(s), corticosteroid nasal spray |
| Gastroesophageal reflux | Bed head elevation, light dinner, diet modification, H2 blockers, omeprazole, metoclopramide |
| ACE inhibitor associated cough | Switch on to losartan |
 howMed Know Yourself
howMed Know Yourself





very useful….thank you…