Cancer chemotherapy includes the drugs used to treat neoplasms, tumors or cancers. These include:
- Antineoplastic agents
- Anticancer drugs
- Cytotoxic drugs
Cancer, neoplasm or tumor is defined as:
“Disease characterized by loss of normal control over cell division and proliferation or differentiation.”
Tumor stem cells are subpopulation of malignant cells which have the capability of further dividing, proliferating or differentiating. There are two types of cells:
- Those differentiated fully –can’t proliferate
- Those which can proliferate further, the stem cells, also have the capability to travel to distant organs, colonize and produce new growth known as metastasis.
Cancer Chemotherapy is different because:
- In others, organisms are foreign to the body structure, thus anti-microbial agents can be given having less side effects to human cells
- Body itself starts immune response against bacteria, viruses but in cancer cells, because these are human cells, body does not feel need of defense mechanism.
- Drugs used affect normal cell machinery and lots of toxic effects are produced.
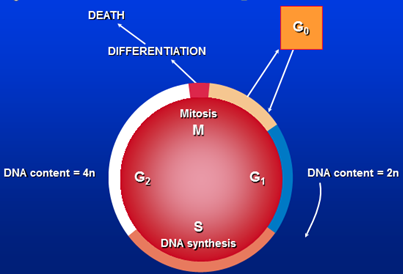
The Cell Cycle
Causes Of Cancer
- Age / sex / race
- Unknown
- Genetic association
- Oncogenes (bcl-2) : genes which predispose a person to developing cancer, found to be overexpressed in certain cancers.
- Tumor suppressor genes (p53) : seen mutated in many types of cancers
- Environmental / occupational
- Tobacco smoke
- Exposure to chemicals, benzene, asbestos
- Exposure to ionizing radiations
- Biological agents –viruses, e.g. hepatitis B and C with hepatocellular carcinoma
- Diet –excessive use of BBQ food, less intake of fiber à colorectal cancer
- Iatrogenic –certain drugs, anticancer drugs like alkylating agents cause blood cancers
Management
Prevention
- Primary
- Lifestyle modificatin
- Risk factors avoidance
- Secondary
- Screening
- Early detection & diagnosis
Treatment modalities
- Surgery
- Radiotherapy
- Chemotherapy
- Stem cells transplantation
- Psychotherapy
Antineoplastic Agents
Approaches
- Primary induction –no other modality other than anti cancer drugs, (palliative )
- Neoadjuvant (curative) –cancers where antineoplastic treatment is given but other modalities are used like surgery, radiotherapy for complete cure.
- Adjuvant –in this alone surgery or radiotherapy is not effective, antineoplastics are added to increase survival and decrease recurrence.
Evaluation of response
- Sign / symptoms
- Size
- Lab diagnostics / markers
Cell cycle kinetics – gompertzian growth
When progression to cancer occurs, malignant cells keep on increasing in number, one way is exponential growth like in leukemias. But in solid tumors or neoplasms, maximum growth fraction is seen when size of neoplasm is about 37% of its overall size. After that availability of blood supply and metabolites goes on decreasing.
Although size increases but fraction of cells is less, called Gompertzian growth.
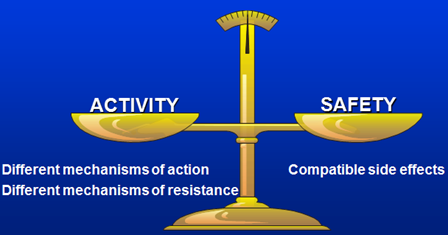
Combinations*
- Efficacy of therapy is enhanced
- If resistance develops to one agent other may act
- All act by different mechanisms
- Adverse effects are decreased
Aim of combination therapy
Efficacy / / toxicity
Principals For Effective Combinations
- Efficacy
- Toxicity
- Optimal Scheduling
- Mechanism of Interaction
- Avoidance of Arbitrary Dose Changes
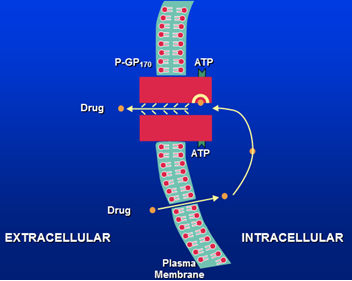
Drug Resistance
- Primary –inherited, most cases p53 gene mutations
- Acquired –in most cases MDR 1 gene is responsible for expression of p-glycoprotein 170, efflux pumps are overexpressed and drug enters cells but is not effluxed out.
General Toxicity
- Bone marrow
Action is more on rapidly multiplying cells, thus cells of bone marrow are affected more which may lead to granulocytopenia, thrombocytopenia, etc.
- Lymphoreticular tissue
Decrease in WBCs, increased chances of infection, increased risk of bleeding
- GIT
Nausea, vomiting, due tooth mechanisms:
- Local irritation of GIT
- Stimulation of vomiting center contrally
- Gonads
- Oligospermia,
- anovulation,
- amenorrhea
- Skin
- Nephrotoxicity
- Neuropathy
- Cardiotoxicity
- Pulmonary toxicity
- Hyperurecemia –when rapid turn over
- Carcinogenicity
- Pregnancy –fetal toxicity and abortion
Management
- Pulses / courses– 3to 4 weeks interval to recover
- Combinations –less doses are given
- Local administration –intra arterial, intra peritoneal, intra pleural route
- Antiemetics added
- Biological response modifiers (erythropoietin, colony stimulating factors)
- Specific treatment:
- Mesna with cyclophosphamide
- folic acid with methotrexate
- allopurinol in blood cancers
Classification Of Antineoplastic Drugs
Chemical Classification
I. Alkylating Agents –most commonly used
a. Classical
- Cyclophosphamide
- Melphalan
- Chlorambucil
- Busulfan
- Carmustine
- Lomustine
- Thiotepa
b. Non-classical
- Procarbazine
- Dacarbazine
c. Platinum Analogs
II. Anti-Metabolites
a. Folic Acid Analog
b. Purine derivatives
- 6 Mercaptopurine
- 6 Thioguanine
- Azathioprine
- Fludarabine
c. Pyrimidine derivatives
- 5- Flourouracil
- Cytarabine
I. Antitumor Antibiotics
- Daunorubicin
- Doxorubicin
- Epirubicin
- Idarubicin
- Mitoxantrone
b. Miscellaneous
IV. Vinca Alkaloids
V. Epipodophyllotoxins
VI. Taxanes
VII. Camptothecins
VIII. Hormones & Anti-hormones
a. Hormones
- Estrogen
- Glucocoticoids
- Progestins
- Androgens
b. Anti-hormones
- Anti-estrogen – Tamoxifen
- Anti-androgen – Flutamide
- GnRH agonist – Goserelin / Leuprolide
- GnRH antagonist – Abarelix
- Aromatase inhibitor – Anastrozole
– Aminoglutethimide
IX. Miscellaneous
a. Asparaginase
b. Retinoic acid derivatives
c. Monoclonal antibodies
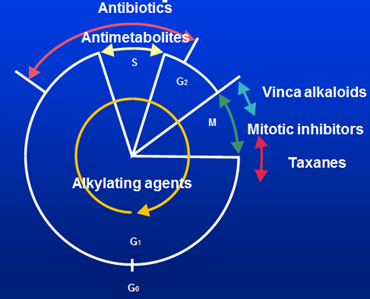
On Basis of Cell Cycle Specificity
A. Cell Cycle Specific (CCS)
I. Anti-Metabolites
a. Folic Acid Analog
b. Purine derivatives
- 6 Mercaptopurine
- 6 Thioguanine
- Azathioprine
- Fludarabine
c. Pyrimidine derivatives
- 5- Flourouracil
- Cytarabine
II. Vinca Alkaloids
III. Epipodophyllotoxins
IV. Taxanes
V. Antitumor Antibiotic
B. Cell Cycle Non-Specific Drugs (CCNS)
I. Alkylating Agents
a. Classical
- Cyclophosphamide
- Melphalan
- Chlorambucil
- Busulfan
- Carmustine
- Lomustine
- Thiotepa
b. Non-classical
- Procarbazine
- Dacarbazine
c. Platinum Analogs
II. Anthracyclines
- Daunorubicin
- Doxorubicin
- Epirubicin
- Idarubicin
- Mitoxantrone
III. Antitumor antibiotics
IV. Camptothecins
V. Hormones & Anti-hormones
a. Hormones
- Estrogen
- Glucocoticoids
- Progestins
- Androgens
b. Anti-hormones
- Anti-estrogen – Tamoxifen
- Anti-androgen – Flutamide
- GnRH agonist – Goserelin / Leuprolide
- GnRH antagonist – Abarelix
- Aromatase inhibitor – Anastrozole
– Aminoglutethimide
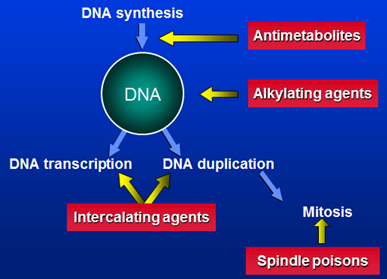
Sites Of Action Of Cytotoxic Agents
Cell cycle level
Cellular level
Continue Reading
Methotrexate, 5-Fluorouracil, Purine Antagonists and Antibiotics Used in Cancer Chemotherapy
 howMed Know Yourself
howMed Know Yourself