Cephalosporins are the derivatives from fungus cephalosporium, cultured near sea.
Classification
Classified into four generations depending upon antibacterial spectrum.
1st generation —— more effective against gram positive bacteria
2nd generation—— more effective against gram negative and less against gram positive bacteria
3rd generation——- no activity against gram positive bacteria
4th generation——- no activity against gram positive, effective against gram negative only
First Generation
- Gram positive organisms,
- Klebsiella,
- Proteus (non indole positive only)
- E coli.
Parenteral
- Cephalothin,
- Cefazolin
Oral
- Cephalexin,
- Cephradine
Second Generation
- Gram positive organisms,
- Klebsiella, (including those resistant to Ist Generation)
- Proteus (including indole positive)
- H. influenzae
Parenteral
- Cefuroxime,
- Cefamandole,
- Cefoxitin
Oral
- Cefaclor,
- Cefuroxime Axetil
Third Generation
Gram negative organisms including
- Citrobacter
- Acinetobacter,
- Serratia,
- Providencia
- Enterobacter,
- Salmonella
Pseudomonas is sensitive only to ceftazidime & Cefoperazone
Parenteral
- Ceftriaxone,
- Cefotaxime,
- Ceftazidime,
- Ceftizoxime,
- Cefoperazone
Oral
- Cefixime
Fourth generation
- Cefepime
Also effective against pseudomonas aerogenosa having the same spectrum as that of 3rd generation except that it is effective against resistant organisms of 3rd generation.
Most of the 3rd generation drugs are effective against pseudomonas.
Chemistry
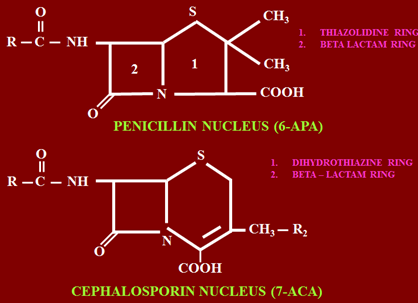
Penicillin contains 5 member thiazine ring bound with beta lactam. Here 6 member dihydro thiazine ring (sulphur containing) bound with beta lactam is present. Rest of the structure is same.
Amide group at position 6 contains R, where substitutions are made.
- Cephamycins: Methoxy group at position 7
- Oxycephems: Sulphur at position 1is replaced by an oxygen
- Carbacephems: sulphur is replaced by carbon
Uses are similar to 3rd gen cephalosporins, differ in structure.
Mechanism of Action
Same as that of penicillins.
- Have bactericidal action
- 1st bind penicillin binding proteins or transpeptidase enzyme, acting as receptors for these drugs, after binding interfere with synthesis of cell wall (peptidoglycan synthesis –transpeptidase reaction).
- Activation of autolytic enzymes –murin hydrolases which damage cell wall.
Mechanism of resistance
- Alteration in penicillin binding proteins
- Less penetration of drug into bacteria esp. which contain lipopolysaccharide layer or other effectors
- Failure of activation of autolytic enzymes
- There is synthesis by bacteria of enzyme beta lactamase known as cephalosporinase, causing break down of beta lactam
Pharmacokinetics
Given both parenteral or orally. Mostly parentally as used mainly against resistant infections.
After absorption well distributed in body compartments, having good penetration in soft tissues, muscles, bones and joints. These drugs can also cross placenta and enter fetal circulation.
Both penicillins and cephalosporins are safer in pregnancy. Also attain high concentration in aqueous humor. Also have high concentration in various peritoneal, pericardial and synovial fluids.
Most of these drugs are excreted unchanged in urine by tubular filtration and secretion.
Ceftriaxone, Cefamandole and Cefoparozone are excreted in feces (bile) thus are safer in patients suffering from renal failure.
Some of these drugs cross BBB, effective in meningitis. Drugs which cross BBB include:
- Cefotaxime
- Ceftizoxime
- Ceftriaxone
PPB of most drugs is variable, in 15-90% range.
Half life of these drugs ranges between 1-4 hours except Ceftriaxone, which is longer (8.5 hours)
Clinical Uses
As are quite expensive, they are reserved for infections resistant to penicillin. They should not be used for ordinary infections.
First Generation
Having narrow spectrum, used in:
1. Surgical prophylaxis (Cefazolin)
2. UTI –uncomplicated by E. coli
3. Chronic bronchitis
4. Skin and soft tissue infections
Alternative to Penicillins
Second Generation
Having extended spectrum, used in:
- H influenzae infections,
- Staph. aureus,
- Strept. pneumoniae e.g. sinusitis, Otitis media, pneumonia
- B fragilis infections (cefoxitin, cefotetan)
- Community acquired pneumonia (cefuroxime)
Third Generation
- Infections by enterobacteria B fragilis (in combination with metronidazole)
- Biliary tract infections or biliary sepsis
- Surgical prophylaxis and post surgical infections
- UTI caused by pseudomonas, instruments or hospital acquired
- Gonorrhea (Cefotaxime, Ceftriaxone), gonorrheal urethritis –drug of choice is penicillin, used only in resistant or hypersensitive cases
- Enteric fever (Cefoperazone, Ceftriaxone) -2nd line drug. Quinolones are 1st line in enteric or typhoid fever
- Nosocomial infections –hospital acquired, difficult to treat
- Serious Gram negative infections (neutropenic infections)
- Meningitis (Cefotaxime, Ceftriaxone, Ceftizoxime) –as cross BBB
- Bacterial endocarditis –in patients not responding to penicillins, given parentally, sometimes combined with aminoglycoside
- Prophylaxis/treatment in immunocompromized patients –as infection is resistant to common antibiotics
- Pseudomonal infections (ceftazidime)- Cefipine (4th gen) may also be used
Adverse Effects
1. Hypersensitivity
Cross allergy may occur when using in hypersensitive individuals, care should be taken. Incidence of cross allergy is between 6-18%, as share beta lactam ring with penicillins. Even anaphylactic reaction may occur
2. Local pain and irritation (I/M)
3. Phlebitis (i/v) –inflammation of vein
4. Nephrotoxicity
Most important adverse drug reaction. Most of these drugs if used for prolonged periods may cause interstitial nephritis as excreted in urine.
5. Hypoprothrombinaemia –drugs containing methyl thiazolidine group having anti vitamin K effect. Treatment is vitamin K, 10 mg twice weekly.
6. Disulfiram like reaction
Disulfiram is used for alcohol aversion therapy. Mainly alcohol is metabolized by aldehyde dehydrogenase. Aldehyde is converted into acetic acid by aldehyde dehydrogenase. Disulfiram inhibits this enzyme increasing plasma levels of acetaldehyde. Patient feels symptoms like headache, flushing, nausea, vomiting due to accumulation of acetaldehyde.
7. Super infection
Very important in 2nd and 3rd generation antibiotics. Especially clostridium difficile, overgrowth of gram positive organisms in intestine causing pseudomembranous colitis and severe diarrhea. Treatment is vancomycin.
8. Thrombocytopenia, neutropenia, interstitial nephritis, abnormal LFTS – May occur rarely if continued for more than two weeks.
Drugs metabolized in liver like Cefoperazone and Ceftriaxone may damage liver.
 howMed Know Yourself
howMed Know Yourself





Recently, there’s news about a death of a man caused by alcohol intoxication. He ate a lot of durian and immediately after that he drank coke. This led to to his death. I’ve read an article in one website that durian contains a lot of sulphur and could impair the alcohol dehydrogenase (alcohol breakdown).
Meaning to say, if someone consume this type of cephalosporin which could impair the alcohol metabolism, he can’t consume highly caffeinated drinksn like coke. Because that would cause sudden intoxication. Does it make sense?