Drug interactions may create alarming situations. In most cases, monotherapy is preferred but sometimes drugs need to be given in combination e.g. in treatment of congestive cardiac failure, diuretics and vasodilators need to be combined, or in patients suffering from malignancy, coma, chemotherapy or tuberculosis. The aim is to:
- Reduce dose
- Prevent the development of resistance
Definition
When pharmacological action of a drug is altered by concurrent administration of another drug.
The adverse drug interactions may be of great clinical importance when margin of safety of drugs is small.
Sometimes clinicians allow drug interactions to occur for better actions, but adverse reactions occur with drugs having low therapeutic index.
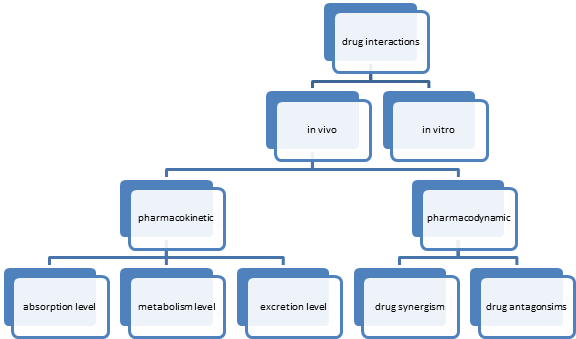
Types
1. In Vitro
2. In Vivo
Drugs interactions can occur outside the body, e.g.
1. Incompatibilities of drug in an IV infusion
2. Use of wrong vehicle for infusion:
a) no drug should be added to blood plasma, aminoacid solutions, fat emulsions, sodium bicarbonate solution, mannitol solution (mannitol may crystalize) and to heparin infusion.
b) Mannitol should not be mixed with electrolytes, KCl or other drugs
Highly acidic solution such as dextrose, or fructorse are unsuitable as vehicle for sodium and potassium salts of weakly acidic drugs. Such as sulfonamides, barbiturates, methicillin and novobiocin
Benzyl penicillin, ampicillin, heparin and aminophylline are unstable at the pH of these solutions.
Isotonic saline is slightly acidic or neutral and is suitable vehicle for most drug like phenytoin, diazepam
Most antibiotics become unstable and deteriorate in large volumes of fluids exceptions are amphotericin B and erythromycin.
Erythromycin lactobionate is unstable in electrolyte solution but may be diluted with 5% dextrose solutions
Amphotericin B should be diluted with 5% dextrose
Calcium salts should not be added to sodium bicarbonate
Incompatibilities in syringe
Soluble and protamine zinc insulin: soluble insulin interacts with excess of zinc and protamine and its onset of action may be delayed
Barbiturates,, phenytoin, phenothiazine, frusemide should not be mixed with any other drug in solution
Penicillin is incompatible with gentamicin, tetracycline and hydrocortisone
Tetracycline is incompatible with calcium salts
Heparin sodium is incompatible with gentamicin and hydrocortisone
Thiopentone sodium is incompatible with succinylcholine
In Vivo
Pharmacokinetic Drug Interactions
Differences in plasma levels of a drug achieved by a given dose of that drug.
Pharmacodynamic Drug Interactions
Differences in pharmacological effects produced by a given plasma level of a drug
Pharmacokinetic Drug Interactions
Drug absorption e.g. antacids
Interactions due to changes in protein binding of drugs – distribution (if highly protein bound, displace other drugs, free levels increase, leading to toxicity)
Interactions affecting drug metabolism
Interactions affecting renal excretion of drugs
Interactions Affecting Absorption
Parenteral administration
Drugs + Epinephrine
Drugs + Methacholine (vasodilator –effective drug levels not achieved)
Oral administration
Chelation / Adsorption
Tetracycline + Ca++
Cholestyramine (adsorption) + Cardiac Glycosides
Sucralfate adsorbs, cannot give other drugs
Altered Intestinal Motility
Atropine + Acetaminophen
Metoclopramide (prokinetic) + Cimetidine (anti ulcer) (increased gastric emptying, less drug absorbed)
Inhibition of Absorption
Phenytoin and oral contraceptives + Folic acid
Colchicine + Vit B12
P-glycoproteins in intestinal wall can influence absorption, present in different cells of body, some drugs may be expelled out.
Influence of Diet
Food in Stomach
Fatty Meal
Griseofulvin has increased absorption with fally meal -EXCEPTION
pH Dependent Absorption
Weak acidic drugs e.g. NSAIDS
Weak basic drugs
Interactions Affecting Distribution
Competition for Plasma Protein Binding
Sulfisoxazole and Bilirubin (may lead to kernicterus)
Displacement from Tissue Binding Sites
Phenylbutazone and Warfarin (displace, also at level of metabolism, thus vitamin K dependent factors are impaired)
Methotrexate + Aspirin (efficacy decreased, PG inhibition, increased levels of methotrexate) so aspirin is stopped before treatment otherwise may cause methotrexate toxicity
Interactions Affecting Metabolism
Monoamine oxidase inhibitor –beneficial effect
Xanthine oxidase inhibitor (allopurinol) –beneficial effect
Enzyme inducers –adverse effects, therapeutic failure, diminished response
Interactions Affecting Excretion
Probenecid with penicillin and methotrexate
Aspirin with methotrexate
Agents that alkalinize urine –weak acid poisoning sodium bicarbonate given
Agents that acidify urine
Pharmacodynamic Drug Interactions
Receptor site down regulation or upregulation
Synergism
Sulfamethoxazole & Trimethoprim
Levodopa with Carbidopa
Antagonism
Rifampicin and Cloxacillin
Protamine and Heparin
Combined Toxicity
Ethanol with opioids, barbiturates and benzodiazepines
 howMed Know Yourself
howMed Know Yourself