Penicillins have made revolution in chemotherapy. They were discovered in 1929 by Alexander Fleming. He noticed colony of Staphylococci, which was contaminated with Penicillium notatum. Later on, penicillins were available commercially in 1949.
Benzyl penicillin was first discovered. Its modification by chemists has led to large number of drugs which are used because of cost-effectiveness.
Chemistry
Penicillins contain thiazolidine ring. 5 member S containing thiazolidine ring is linked with beta lactam ring. At R amide group is present. Substitution can be made:
- When substitution is with benzyl group, we get benzyl penicillin
- When substitution is with amino group, we get amino penicillin
- When substitution is with phenoxy methyl group, we get phenoxy methyl penicillin
Position 6 has amide group.
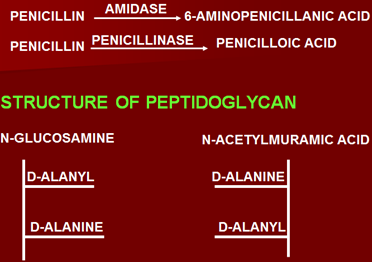
If penicillin is degraded, 2 types of enzymes are involved:
- Amidase -6 amino penicillamic acid
- Penicillinase or Beta lactamase –Peniciloic acid (which has antigenic properties and is allergic)
Mechanism of action of penicillin:
Act by inhibiting/interfering synthesis of cell wall in bacteria. Actually interfere with the synthesis of last step in cell wall i.e. synthesis of peptidoglycan.
Structure of peptidoglycan
- Polysaccharides: 2 polysaccharides, Glucosamine and N-acetyl muramic acid.
- To these are attached penta peptides –D alanyl and D alanine
They are linked to each other by transpeptidation by enzyme transpeptidase.
Site of action
Inhibit transpeptidase enzyme, inhibiting transpeptidation. Holes are created in the cell wall of bacteria.
Accomplished by:
- Penicillins are mainly effective against rapidly growing organisms (cell wall)
- Safer in human beings (as have no cell wall)
- Binding to penicillin binding proteins (bind transpeptidase enzyme)
- Inhibition of transpepditation
- Activation of autolysins or murinhydrolases, forming holes in cell wall.
- Action is mainly bactericidal
Mechanism of resistance
- Altered penicillin binding proteins or of higher molecular weight having less affinity for drug
- Inability to penetrate
Certain bacteria are gram negative covered by lipopolysaccharide membrane. Certain drugs cannot penetrate. Benzyl penicillin cannot penetrate but certain amino penicillins can easily penetrate outer membrane. Membrane can decrease the entry of bacteria.
- Production of beta lactamase or penicillinamase by gram negative bacteria, breaking down beta lactam.
- Failure of activation of autolytic enzymes
- Lack of cell wall like mycobacteria and certain l forms of bacteria
- Intracellular organisms are not affected.
Main mechanisms are the altered PBPs and production of beta lactamase.
Classification
Natural penicillin & related drugs
- Benzyl penicillin,
- Phenoxymethyl penicillin
- Benzathine penicillin,
- Procaine penicillin
Semisynthetic
Β– lactamase resistant (Against β– lactamase producing Staphylococci)
- Methicillin,
- Oxacillin,
- Cloxacillin,
- Flucloxacillin
Extended spectrum
Aminopenicillins (against E. coli & H. Influenzae)
- Amoxicillin (alone & with clavulanate)
- Ampicillin (alone and with sulbactum)
Carboxypenicillins (Against pseudomonas, enterobacter & proteus spp)
- Carbenicillin,
- Ticarcillin
Ureido penicillins (against pseudomonas, klebsiella & gram negative organisms)
- Azlocillin,
- Mezlocillin
- Piperacillin (alone and with tazobactum)
Pharmacokinetics
- Benzyl penicillin is given mainly parentally as destroyed by gastric acids.
- Amino penicillins are resistant to acids and are given orally, thus they differ from others.
- As bind food, given one hour before or two hours after meals.
- Others like carboxy penicillins and urido penicillins are given parentally.
- After absorption penicillins are distributed to all body compartments well. Penetration of CSF is very low in normal meninges (1% of plasma levels). When inflamed, entry increases to 5%.
- These are mainly excreted in urine, thus dose has to be reduced in renal insufficiency.
- Excreted by 90% tubular secretion and 10% by glomerular filtration
- Probenecid (uricosuric agent) if given along with penicillin, increased plasma levels of penicillin occur as it competes for tubular secretion.
- If older days small quantities of penicillin were available, now huge amounts are manufactured, thus there is no need of Probenecid. It is used only if very high levels are required like in endocarditis.
- Single injection is given for gonorrhea.
- It is also excreted in sputum and milk ranging from 5-15%.
- Very small amount is metabolized in liver.
- Long acting preparations of benzyl penicillin are available with half life of 2 hours.
- Long acting penicillins include procaine (effective plasma conc. Up to 24-48 hrs.) and benzathane (up to one month)
Benzyl penicillin
1st drug discovered and used where very high plasma concentration of drug is required.
Spectrum of activity
It is effective against gram positive and some gram negative bacteria.
Gram positive cocci
- Streptococci,
- pneumococci,
- staphylococci (non beta – lactamase producing)
Gram negative cocci
- Meningococci,
- Gonococci
Gram positive bacilli
- Bacillus anthracis,
- Corynebacterium
- Diphtheriae,
- Clostridia
Spirochetes
- Treponema pallidum,
- Fusospirochetes
Others
- Actinomyces Israeli
- Pasturella multocida
- Listeria monocytogenes
- Erysepella infection
Uses of benzyl penicillin
- Treatment of beta hemolytic streptococcal infections such as acute tonsillitis, acute pharyngitis, skin infections, bone infections
- Pneumococcal infections such as pneumococcal pneumonia, pneumococcal meningitis (massive doses)
- Meningococcal meningitis (massive doses)
- Staphylococcal infections (non beta – lactamase producing strains only)
- Anaerobic infections (excluding those caused by b. Fragilis)
- Syphilis
- Actinomycosis
- Anthrax
- Leptospirosis (Weil’s disease)
Pharmacokinetics
Benzyl penicillin is mainly given I/V or by I/M route.
Dose is in range of 300-600 mg 6 hourly. In case of infections which are very severe or localized, like endocarditis, benzyl penicillin is given in very high doses of 7.2-14.4 g in the form of long acting preparations.
Benzathine penicillin and Procaine penicillin
Benzathine penicillin (benzyl penicillin combined with ammonium base having effective plasma conc. for about one month) or procaine penicillin are used in treatment and prophylaxis of rheumatic fever, given as a single dose I/M with injection of 1.2 million units.
In case of prophylaxis of rheumatic fever 1.2 million units are given every month.
It is also used in treatment of syphilis in dose of 1.2-2.4 million units I/M.
Long acting penicillins are always given I/M.
Procaine penicillin consists of procaine (local anesthetic) combined with penicillin to delay absorption from I/M site, resulting in prolonged duration of action. It plays two major functions:
- Mainly delays absorption of benzyl penicillin from site of action
- Decreases pain
In treatment of gonococcal infection 4.8 million units single injection should be given I/M.
Phenoxy methyl penicillin
It differs from benzyl penicillin in chemistry; having phenoxy benzyl group at R. it can be given by oral route as resists acids in stomach.
Drug in antibacterial spectrum has less action against gram negative organisms especially Neisseria. It is mainly used in children especially to treat minor infection esp.
- respiratory tract infection
- Otitis media
- Also used for maintenance therapy once the infection is controlled by benzyl penicillin, as can be given orally.
Dose is 250-500 mg 4 times daily.
Semi synthetic
Beta lactamase resistant
Methicillin –not used because of toxicity and resistance
Oxacillin,
Cloxacillin,
Flucloxacillin
Oxacillin
Differs in that
Chemistry
Chloride atom –Cloxacillin
Chloride + fluoride in place of hydrogen –flucloxacillin
Since these are resistant to beta lactamase enzyme, they contain acyl group in structure which protects beta lactam bond.
It can be given orally. Food interferes with absorption thus should be given one hour before or two hours after food (except methicillin). Have extensive PPB up to 90%.
Uses
Treatment of Staphylococcal infections or those of beta lactamase producing staphylococcal infections.
Dose 250-500 mg/6 hourly.
Although methicillin is not used, but can be used in labs to test the sensitivity of bacteria against antibiotics. Bacteria resistant to methicillin are resistant to all other beta lactamase antibiotics, known as MRSA (methicillin resistant staph. Aureus). Special group of antibiotics is used to treat infections by Staph. Aureus.
Amino penicillins
Chemistry
Amino group is present at R and differs from benzyl penicillin in antibacterial spectrum in that it is extended spectrum
In addition to the spectrum of benzyl penicillin are effective against:
- E. coli
- H. influenza
- Typhoid infection (Salmonella)
- Shigella
These drugs can also be given by oral route. Food interferes with
Absorption, thus given 1-2 hours after meals. These drugs are ineffective
Against beta lactamase, thus combined with beta lactamase inhibitors like Clavulanate, Salbactum which inhibit beta lactamase enzyme.
Uses of amino penicillin
Mainly used against gram negative and positive infections. Main uses are:
- Upper Respiratory Tract Infection
Especially of gram negative organisms, H. influenza, also gram positive infections
- UTI (2nd choice)
Especially caused by E. coli
- Meningitis
Especially that of Neisseria and H. influenzae
- Salmonella infection (2nd choice)
Enteric fever
- Bacillary dysentery (2nd choice)
Ampicillin is mostly used as is rapidly absorbed from GIT, but less than amoxicillin
Some of these drugs like Becampicillin, which is a prodrug, and is converted into ampicillin during absorption from intestines. Talampicillin is also a prodrug.
Because amoxicillin is rapidly absorbed, it is given 3 times daily. Dose is 250-500 mg. ampicillin is given four times daily.
Carboxy penicillins
Carboxy penicillins differ in that they are also effective against pseudomonas and proteus species. Most commonly used are Carbenicillin and Ticarcillin. They are always given by parenteral route.
Mainly used for treatment of infections by these organisms, mainly:
- UTI,
- Bacteremias
- Post surgical infections
- Sepsis
Of these carbenicillin is cost effective.
Main disadvantage is that they are given in very high doses of about 10-30 g 4 times daily. Important is the fact that these drugs are available in the form of sodium salts thus are contraindicated or used very carefully in patients suffering from hypertension, cardiac and renal disease.
Ticarcillin is 4 times more potent than carbenicillin and is also used in less doses of about 4-12 g.
Ureido penicillins
- Have same spectrum as carboxy penicillins but differ in that they are derivatives of ampicillin with a urea side chain
- Are 8 times more potent than carboxy penicillins
- Safer in patients of renal diseases.
- 25% of these are excreted in bile.
- On dose increment may follow zero order kinetics
- Piperacillin is active against anaerobic infections
Adverse effects of Penicillins
1. Hypersensitivity reactions
a. maculopapular rash
Mostly common with ampicillin especially when given to patient suffering from lymphatic leukemia, viral infectious disease known as infectious mononucleosis.
b. urticaria
c. angio edema (laryngeal obstruction, respiratory distress)
d. serum sickness (fever, joint pains, lymphadenopathy)
e. exfoliative dermatitis
f. Stevens Johnson syndrome
g. Anaphylaxis
Especially with parenteral penicillins, most important and lethal adverse drug reaction. Thus when using penicillins especially benzyl penicillin test dose is given first.
If occurs, adrenaline is the treatment given.
2. Phlebitis (I/V)
3. Local pain and inflammation (i/m)
4. Degeneration of nerve (radial or sciatic)
Because when administered I/M in upper hand, damage to radial nerve may occur.
When given in buttocks, damage to sciatic nerve may occur. Precautions have to be taken. Patient is asked to bend arm, groove of radial nerve is seen, and then injection is given in upper or lower end. In buttocks, given to upper and side of buttocks.
5. Neurotoxicity
Especially after intrathecal administration as may cause irritation of nerves especially in patients of epilepsy.
6. Super infections
Penicillins having extended spectrum have more activity against gram negative organisms, esp. ampicillin also has local action causing growth of gram positive organisms like Clostridium deficile which will cause pseudomembranous colitis in intestine, leading to severe diarrhea after intake of ampicillin.
Also occurs with tetracyclines and quinolones having broad spectrum.
Treatment of super infections is administration of Vancomycin or metronidazole.
7. Hemolytic anemia (benzyl penicillin, massive doses)
8. Renal damage (methicillin) –not used now, only in labs
9. Hypokalemic alkalosis
10. Defects in hemostasis – with carbenicillin
Uses in dentistry
- Dental plaque (Streptococcus mutans)
- Dental caries(strept mutans, lactobacilli)
- Periodontal disease/ gingivitis (anaerobes, gram – ive rods)
- Acute bacterial sialoadenitis
- Sialolithiasis
- Ludwigs’ angina
- Sublingual/submandibular cellulitis
- Acute glossitis
- Cancrum oris
Drug interactions
1. Salicylates
Can increase the effects of penicillins by displacing them from protein binding sites, when administered together.
2. When given with bacteriostatic antibiotics, decreased activity of drugs. Bactericidal drugs are only effective against rapidly growing bacteria. Bacteriostatic drugs inhibit growth.
Penicillin is not combined esp. with chloramphenicol and tetracyclines.
Can be combined with bactericidal drugs.
With aminoglycosides commonly used as potentiates effects. Penicillins increase entry of aminoglycosides, having synergistic effects.
But should not be given through same syringe as may lead to inactivation of these drugs.
Dose
Penicillins are given in both mg and units.
Older drugs are given in units while newer in mg.
1 mg = 1667 units
1 mega unit (1 million) of penicillin = 600 mg
 howMed Know Yourself
howMed Know Yourself