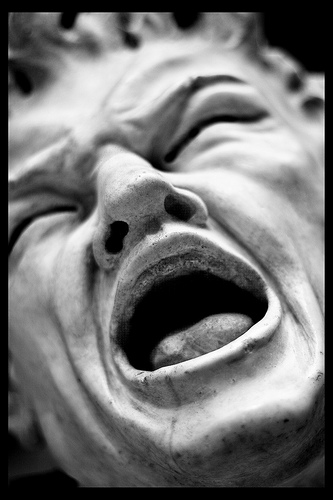
One of the mankind’s oldest and most dreaded fears.
Photo by A. Strakey
Definition:
Neuroscientist:
Pain is a sensory phenomenon registered on “perception”.
Psychologist:
Pain may be a “learned / conditioned behavior”.
Doctor:
“Warning sign” to be decoded for the diagnosis & treatment.
“A sensation of discomfort”
Pain is an unpleasant sensory or emotional experience associated with actual or potential tissue damage.
Nociception is unconscious activity induced by a harmful stimulus applied to sense receptors.
Pain has two functions:-
• Physiologically pain is a protective mechanism.
• Pain acts as a symptom of tissue damage.
Types of Pain:
Two major types;
1. Fast Pain:
“ Sharp pain, Pricking pain, Acute pain, Electric pain”
Felt within 0.1 Sec after application of stimulus (mechanical & thermal stimuli).
Not felt in most deeper tissues of the body.
2. Slow Pain:
“Aching pain, slow burning pain, throbbing pain, nauseous pain, chronic pain”
• Felt after 1 sec or more
• Increases slowly over many secs or mins
• Commonly associated with tissue destruction
• Occurs both in skin & deeper tissues
• Elicited by all the three types of stimuli; mechanical, thermal & chemical.
“Nociceptors” or Pain Receptors
All types of pain receptors are “free nerve endings”.
Widespread in superficial layers of skin & deeper tissues e.g. Periosteum, Arterial walls, Joint surfaces, Falx & tentorium in cranial vault
Non-adapting nature of pain receptors:
Adapt very little or not at all.
May be due to increased sensitivity of pain receptors (Hyperalgesia).
Keeps the person apprised of damaging stimulus.
Three types of nociceptors:-
1. Mechanical nociceptors :
Respond to mechanical damage, pressure, crushing or cutting.
2. Thermal nociceptors:
Respond to extremes of temperature.
3. Chemical nociceptors:
Respond to chemicals released from damaged tissues
* Bradykinin * Acids
* Serotonin * Ach
* Histamine * Proteolytic enzymes
* Potassium ions * Lactic acid
Prostaglandins & Substance P enhance the sensitivity of pain endings and do not directly excite them.
Mechanism of Pain Production
1. Tissue Damage:
Perception of pain begins e.g. when skin heated above 45 0 C; tissues begin
to damage.
Intensity of pain is closely related with the rate of tissue damage by;
e.g. Heat, infection, tissue ischemia, tissue contusion etc.
2. Tissue Ischemia:
3. Muscle spasm: “common cause of clinical pain syndromes”
a. Direct effect: stimulation of mechanosensitive pain receptors
b. Indirect effect: compression of tissue blood vessels & ischemia
Neurotransmitters of Pain:
1. Glutamate:
* Secreted in spinal cord at Aδ Nerve endings
* Involved in transmission of fast pain into CNS
* Duration for few msec
2. Subs P:
Secreted at C-type of unmyelinated N. fibers in spinal cord
Found in high conc. in Spinal cord & Hypothalamus
Involved in transmission of slow chronic pain
Subs P is released slowly
Builds up its conc. for sec or mins
‘Double pain’ sensation of ‘Pin Prick’
Due to the release of;
(i) Glutamate (Fast pain sensation)
(ii) Subs P (More lagging sensation of pain)
Transmission of Pain Signals into CNS
Two Separate Pathways:-
1. Fast-sharp Pain Pathway: (Neospinothalamic tract)
Transmitted in peripheral nerves to spinal cord & to CNS by Aδ fibers.
Velocity of transmission = 6-30 m /sec
Travel through Neospinothalamic tract in Anterolateral columns to brain.
Fibers of Neospinothalamic Tract terminate as :-
a. A few in Reticular Areas of Brain Stem
b. Mostly pass on to VBC of Thalamus with DCL system
*(Fast-sharp pain can be localized exactly).
c. A few in Posterior nuclear group of Thalamus / Basal Areas of Brain.
d. Somatosensory cortex*.
2. Slow-chronic Pain Pathway: (Paleospinothalamic Tract)
Transmitted by C-fibers @ 0.5-2 m/sec
Poor localization of slow pain
Fibers of paleospinothalamic tract terminate:-
1/4th to 1/10th fibers in thalamus
(Intralaminar/Ventrolateral Nuclei)
Mostly in Reticular nuclei of Medulla, Pons & Mesencephalon
Tectal area of Mesencephalon deep to superior & inferior colliculi
Periaqueductal gray region
Referred Pain
“Feeling of pain in a part of the body that is fairly remote from the tissue causing the pain”.
“Pain originates in a visceral organ but sensed at a somatic site or deep pain referred to the surface of the body”.
Examples;
Angina pectoris: Pain due to ischemia of cardiacmuscle; felt in mid-sternal region, base of the neckand down the left arm.
Pain arising in Gall bladder/Bile ducts: referred to the epigastrium & Rt scapular region.
Pain in diaphragm referred to Rt. shoulder.
Pain in ovaries is felt in umbilicus.
Renal pain referred to loin.
Pain in testes is felt in abdomen.
Mechanism of Referred Pain
i. “Dermatomal Rule”
‘A dermatome includes all the structures or parts of the body which are innervated by afferent nerve fibers of one dorsal root e.g. heart and inner aspect of left arm originate from the same dermatome’.
Pain is referred to the dermatome supplied by the dorsal nerve roots through which impulses from the diseased structure reach CNS.
Pain of the deep organ or viscera is referred to the same dermatome from which it was developed/share nerve supply.
ii. Convergence-projection Theory
Referred pain may be convergence of somatic & visceral pain fibers on the same 2nd order neurons in the dorsal horn that project in thalamus and then to somatosensory cortex.
Somatic & visceral neurons converge in lamina I – VI of ipsilateral dorsal horn but neurons in lamina VII receive afferents from both sides of the body.
Visceral Pain
Pain originating from different viscera of the abdomen and chest due to:- visceral inflammation, visceral infections & ailments etc.
Viscera have “Pain receptors” only.
Visceral Pathway of Pain:
Via pain sensory fibers within autonomic nerve bundles.
Pain is referred to the surface often far from the painful organ.
Parietal Pathway of Pain:
Conducted directly into local spinal nerves from parietal peritoneum, pleura, pericardium.
Sensations are localized directly over the painful area.
Difference Between Surface Pain & Visceral Pain
Localized damage on surface may produce severe pain whereas, localized damage of viscera don’t produce severe pain.
Diffuse stimulation of pain N. endings on larger area of Viscous – produces severe pain.
Pain from viscera is difficult to localize.
Visceral pain from thoracic & abdominal viscera is transmitted through C-fibers (Chronic – aching – suffering type of pain)
 howMed Know Yourself
howMed Know Yourself



helped aloot….thanks