Tumor Diagnosis
1. Imaging:
- X-ray
- Ultrasound
- CT scan
- MRI
2. Tumor markers (may be specific for specific tumors)
- Receptors
- Hormones
- Enzymes
- Other proteins
3. Cytology
- Pap smear (diagnosis of cervical pathology from nature of cells from slide)
- Exfoliative cytology (tumor cells have capacity to shed off inside fluids including peritoneal, pleural fluids, from which they are aspirated and microscopy is performed to demonstrate loss of polarity)
- FNA (fine needle aspiration) or FNAC (fine needle aspiration cytology)
4. Biopsy
Histopathology
5. Molecular techniques
Gene detection
Tumor Markers (laboratory analysis)
- Hormones
- Antigens
- Enzymes
- Proteins
- Mucins detection in blood
- CA -125 –used for detection of ovarian cancer
- CEA –carcinoembryonic antigen –used in colorectal carcinoma
- Alpha fetoprotein –hepatocellular carcinoma
- hCG –human chorionic gonadotropin –choriocarcinoma –used for malignant tumor of placenta
- Immunoglobulin –malignant tumor of bones –used for multiple myeloma
- PSA –prostatic specific antigen –used for adenocarcinoma of prostate
- Catecholamines –used for adrenal cortex
- Calcitonin –malignant tumor of thyroid
Other markers in Body Fluids
- p53, K-ras in stool for colorectal carcinoma
- mutated p53 in sputum for cancer of lung
- mutated p53 in saliva for head and neck cancer
- mutated p53 in urine for bladder cancer.
Cytopathology
Cytopathology is the study of cells for the diagnosis of disease.
Types:
1. Exfoliative
Cell samples are collected from normally shedding tissues like pleural effusion.
Stain used is hemotoxylin/eosin stain or Giesma stain.
Lymphocytes and macrophages are seen in tuberculosis.
2. Non-exfoliative
Cell samples are collected by needles (FNAC) for superficial tumors. Deep tumors cannot be studied.
Sample is fixed in absolute alcohol, hemotoxylin/eosin is applied and observed under microscope.
FNAC
Take appropriate 5cc syringe, smear is made, which is put in container containing absolute alcohol (fixation), stained with hemotoxylin/eosin and observed under microscope.
Used to differentiate between benign and malignant.
Advantages of FNA
- Easy/quick office procedure
- No specialized equipment is required,
- Inexpensive
- Even properly trained lab assistant can take the sample
- It helps to differentiate between benign and malignant lesions.
- Diagnostic and therapeutic in benign cysts.
- Helps patient to plan treatment in case of carcinoma.
Disadvantages of FNA
- In situ vs invasive carcinoma cannot be differentiated
- Vascular or lymphatic invasion cannot be assessed.
- Grading cannot be done
- Complications –bleeding, nerve damage.
- Only cellular morphology is seen, no basement membrane
Biopsy –Histopathology
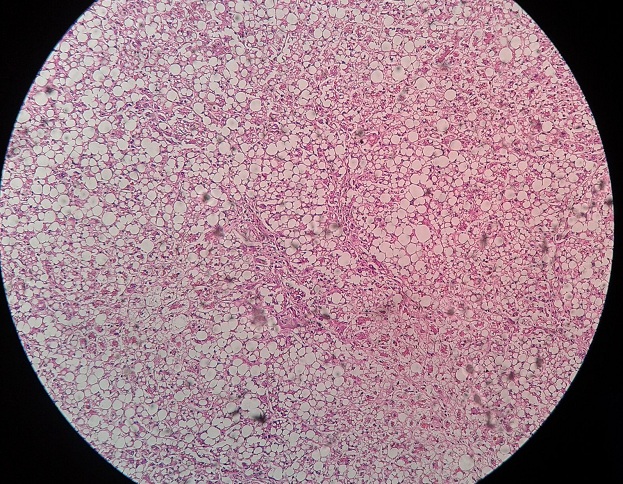
Histopathology
Study of tissue under microscope.
Biopsy
Removal of tissue for diagnostic or therapeutic purpose.
Types
- Aspiration biopsy
- Incisional biopsy (2-3 mm in size)
- Excisional biopsy (both diagnostic and therapeutic purpose, when size of tumor is small whole can be excised)
- Needle biopsy/core biopsy –cylindrical biopsy (taken from organ under ultrasound exam)
Removal of whole mass
Also histopathological exam
Fixation and staining
In fresh form tissues are soft.
- After fixation it becomes easier to take thin slices. 5-10 µm. for this purpose paraffin wax is used.
- To keep the cells in original morphology, so that they can be observed easily
Staining –hemotoxylin/eosin
- PAS (periodic acid Schiff)
- Giesma
- Congo red
Advantages of histopathology
1. Grading can be done
2. Vascular/lymphatic invasion can be determined
3. Can be used for immunostaining
4. Other special stains can be used
5. Excision margins can be determined
To see whether whole tumor has been removed or not –frozen section can also be used
Painted with India ink
If not clear (margins involved), tumor has not been removed completely.
6. Differentiation between primary tumor and metastatic tumor
Frozen Section
Quick procedure like histopathologic exam but no fixation is required, so time is reduced (12-24 hours) with the help of freezing agent (liquid nitrogen) and tissue becomes frozen in 2-3 minutes.
Slide can be made and stained.
- Greezing agent acts as embedding agent by forming minute ice crystals within cells.
- More rapid (5 min)
Freezing microtome is used to cut slices, surgeon is told over phone call whether tumor is benign or malignant.
- Extend margins
- For sentinel lymph node –have to remove others as well
Immunohistochemistry
Specialized procedure used to distinguish between benign and malignant tumors, rather reserved for difficult malignant tumors.
Basic principle
To make the antibody-antigen complex in cells and tissues and making it microscopically visible.
Chromagens are brown in color (99% of the cases), they are made visible when antigen binds antibody.
Uses of immunohistochemistry
- Identification of undifferentiated malignant tumors
- Determination of site of origin in metastatic tumor
- Prognostic significance
- Therapeutic significance
Estrogen receptor antigen –breast cancer slide
Tamoxifen –chemotherapeutic agent used for breast cancer, binds receptors àresponse to chemotherapy is much better.
HER-2 NEU staining
Present over cell membrane –for prognostic significance, positive in aggressive type of breast carcinoma.
Molecular Techniques –gene detection
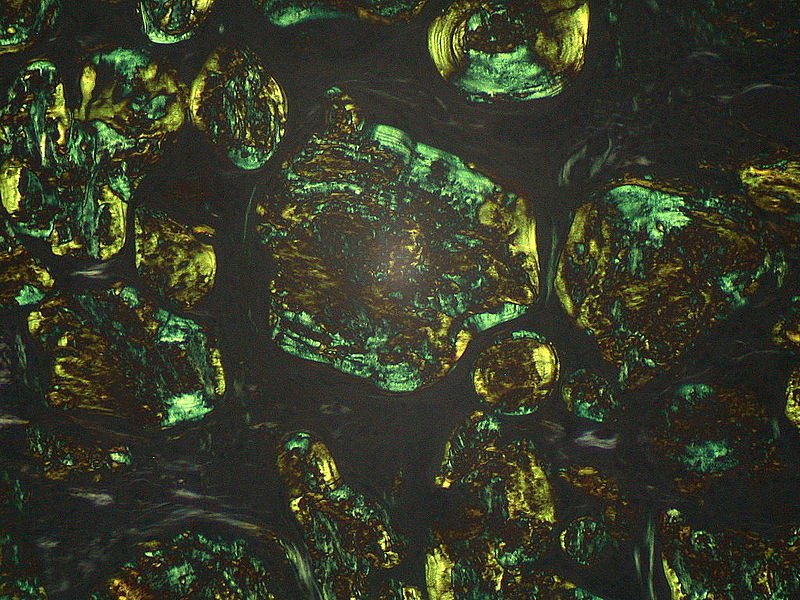
- FISH –fluorescence in situ hybridization
- PCR –polymerase chain reaction
- Spectral karyotyping –chromosomal painting and detection of chromosomal rearrangements
- Comparative genomic hybridization, converted to microarray format
Uses of molecular techniques
1. Diagnosis of malignant neoplasms. Detection of T or B cell receptor in peripheral blood by PCR. Either reactive or neoplastic (lymphomas)
2. Diagnosis of sarcomas
Sarcomas of childhood whose morphology is same. Round blue cell tumors (retinoblastoma, Weln’s tumor)
3. Prognosis of malignant neoplasm
Certain chromosomal alterations are associated with poor prognosis.
If such alterations are present, tumor is more aggressive
If absent, tumor is less aggressive
4. Detection of minimal residual disease
Detection of K-ras mutations in stool after surgical removal if colon cancer either after:
- Surgical removal
- Radiotherapy
5. Detection of hereditary predisposition to cancer
Mutations of certain genes are associated with high risk of associated cancers.
BRCA-1, BRCA-2 in breast cancer, close relatives may develop.
 howMed Know Yourself
howMed Know Yourself