Insulin is a hormone secreted by the beta cells of pancreas, and is important in the regulation of carbohydrate and fat metabolism in the body.
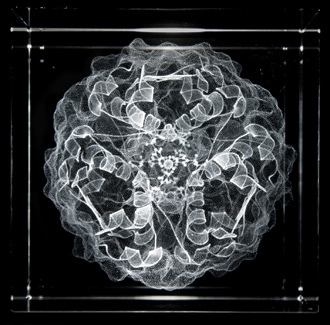
Structure of insulin. Photo by Marie Boran
Discovery:
The discovery of Insulin by Banting and Best in 1922 was a major breakthrough in endocrinology.
Chemistry:
Insulin is made up of 2 polypeptide chains linked by disulphide linkages.
Synthesis:
Insulin is synthesized as preprohormone having molecular weight of 11500. It is converted into proinsulin in endoplasmic reticulum with molecular weight of 9000, and finally into insulin in Golgi apparatus having molecular weight of 5808.
Metabolism
Insulin has a plasma half life of 6 minutes before being broken down catalyzed by the enzyme Insulinase.
Insulin receptor
Insulin receptor is made up of 4 subunits which are linked through disulphide linkages. There are 2 alpha and 2 beta subunits. The 2 alpha subunits are located outside cell membrane and have the insulin binding site. The 2 beta subunits penetrate cell membrane.
Mechanism of Action of Insulin
Mechanism of action can be well understood considering the following points:
1. Binding of insulin with alpha subunit
2. Autophosphorylation of alpha subunit
3. Activation of tyrosine kinase
4. Phosphorylation of intracellular enzymes
Metabolic effects
The metabolic effects of insulin include:
1. Glucose uptake (glucose transport proteins)
2. Amino acid, potassium & phosphate uptake
3. Phosphorylation of enzymes (10-15 min)
4. DNA transcription & RNA translation (hours-days)
Effects of Insulin:
Insulin affects the following:
1. Carbohydrate metabolism
Insulin has profound effects on the following:
a. Skeletal muscles:
Insulin promotes glucose uptake and metabolism by the skeletal muscles. The muscles use fats in the resting state of the body as the membranes are impermeable to glucose; whereas they utilize glucose for a few hours after a meal which is insulin dependent (insulin increases the permeability of membranes to glucose). Also during exercise, contraction of muscles promotes utilization of glucose. Insulin promotes glucose storage by the muscles; therefore, muscles under normal conditions have excess glucose – glycogen stores.
b. Liver
Insulin increases glucose utilization by the liver cells promoting glycolysis and glycogenesis, at the same time decreasing glucose utilization by decreasing glycogenolysis and gluconeogenesis. Excess of glucose that cannot be converted into glycogen is converted into fatty acids.
In between meals, all events are reversed and the glucose is released from liver between meals
c. Brain
Glucose is the only energy source for brain. Glucose permeability of brain cells is insulin independent. Hypoglycemic shock, in which blood glucose concentration is reduced to 20-50 mg/100 ml causes depression of brain functions leading to nervous irritability, fainting, seizures & coma
d. Other cells
In the rest of the cells, insulin increase glucose transport and usage. Glucose is converted into glycerol in adipose tissues and thus insulin promotes deposition of fat.
2. Fat metabolism
Insulin promotes fat synthesis and is thus fat sparer. It stimulates fatty acid synthesis in liver. This occurs by the following mechanism:
1. Inhibition of glycogen synthesis (liver glycogen 5-6%)
2. Activation of acetyl-CoA carboxylase, leading to an excess of citrate & isocitrate ions and conversion of acetyl-CoA to Malonyl-CoA
3. Activation of lipoprotein lipase which splits triglycerides into fatty acids, which are transported into adipose cells and stored.
Fat storage in adipose cells:
This occurs by
1. Inhibition of Hormone Sensitive Lipase which decreases hydrolysis of triglycerides
2. Promotion of glucose transport resulting in synthesis of new fatty acids as well as alpha-glycerol phosphate
3. Protein metabolism
Insulin increase protein synthesis by increasing amino acid transport into the cells as well as by increasing DNA transcription and RNA translation. It also reduces protein catabolism and inhibits gluconeogenesis. Absence of insulin leads to increased protein catabolism and depletion of protein stores which leads to an increase in plasma amino acids. Thus the protein synthesis stops.
Insulin deficiency
Insulin deficiency leads to increased lipolysis by
1. Activation of HSL resulting in increased hydrolysis of triglycerides and increased release of free fatty acids. Thus and increase in plasma free fatty acid levels occurs.
2. An increase plasma cholesterol levels occurs.
3. Excess free fatty acids are converted into phospholipids and cholesterol which increases plasma cholesterol and lipids leading to an increased risk of atherosclerosis.
Ketoacidosis
Increased plasma free fatty acids lead to an activation of carnitine transport mechanism resulting in increased beta oxidation increased plasma levels of Acetyl-CoA. These are converted into acetoacetic acid by ketone bodies formation.
Insulin lack decreases the utilization of acetoacetic acid which is converted into acetone and beta hydroxy
Butyric acid. Increased ketone body formation leads to acidosis, coma and eventually death
Insulin & Growth Hormone acts synergistically:
Insulin and growth hormone act synergistically in promoting growth. They do so by increasing transport of amino acids into the cells. Both cause the transport of different amino acids.
Mechanism of Insulin secretion
Mechanism can be easily understood considering the following points:
1. Hyperglycemia, the stimulus results in
2. Glucose influx via GLUT-2
3. Glucose phosphorylation takes place by glucokinase enzyme, resulting in
4. Formation of ATP
5. Inhibition of ATP-sensitive K channels, increasing positivity inside the cells, causing
6. Membrane depolarization, leading to
7. Opening up of voltage gated Ca++ channels, resulting in
8. Calcium influx, which induces
9. Exocytosis of insulin vesicles
Thus the release of Insulin occurs from beta cells
Other factors which increase insulin secretion:
1. Increased ATP
2. Increased intracellular Calcium mediated by Glucagon, GIP, Acetylcholine etc.
3. Sulphonylurea drugs which bind to ATP-sensitive K channels, resulting in their depolarization.
Diseases:
Insulin has a relation with following disease conditions:
Diabetes Mellitus:
Endocrine disorder characterized by hyperglycemia and disorders of carbohydrate, protein and fat metabolism.
Type I: Decreased production of insulin, early onset diabetes mellitus.
Type II: Decreased sensitivity of cells to insulin, late onset diabetes mellitus.
Insulinoma:
Tumor of pancreatic beta cells causing excess production of insulin leading to hypoglycemia.
Want a clearer concept, also see
 howMed Know Yourself
howMed Know Yourself