Anti-Metabolites
Anti metabolites are used to inhibit different metabolic pathways, as rate of metabolism and required metabolites are much higher for malignant cells.
3 groups are present:
Methotrexate
Mechanism of Action
- Inhibits dihydrofolate reductase – blocks conversion to tetrahydrofolate for synthesis of many cellular components.
- Interferes with synthesis of thymidylate, purine, serine, methionine, proteins, RNA, DNA
Pharmacokinetics
- Given orally, I/V or by intrathecal route
- In cells, it is converted to methotrexate polyglutamate by addition of glutamate residues required for therapeutic effects.
Resistance
- decrease in permeability into cells
- decrease in formation of polyglutamate in cells
- alteration in target enzyme dihydrofolate reductase (decreased affinity or increased production)
- formation of P170 glycoprotein –efflux pumps pump out drug from cells
Uses
1. anticancer (head & neck, breast, CNS, bladder osteogenic sarcoma, NH lymphoma)
2. rheumatoid arthritis
3. psoriasis (autoimmune)
Toxicity
– General / mucositis
– Lucovorin rescue (increased levels of methotrexate lead to leucovorin reduced formation so folates are given, called leucovorin rescue)
5-Fluorouracil
Purine analog
Pharmacokinetics
- Given I/V, it is a prodrug, inside body converted into active metabolites, fluorouridine monophosphate
- Metabolized and dihydropyridine dehydrogenase in some is completely or partially deficient, thus toxicity may be seen.
Uses
– colorectal ( FOLFOX)
– solid tumors (breast, stomach, pancreas, esophagus, liver, head & neck, anus)
Toxicity
- Bone marrow suppression
- GIT toxicity
- Head foot syndrome of skin
- Neurotoxicity
Mechanism of Action & Pharmacological effects
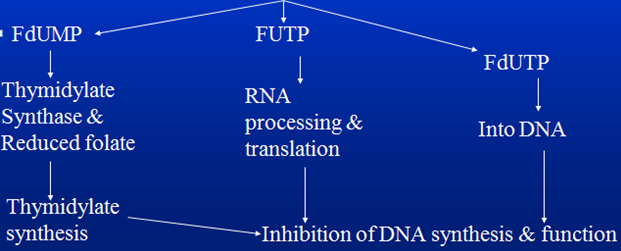
Converted into
Different metabolites affect DNA, RNA, protein synthesis and function.
- One is 5 FdUMP having affinity for thymidylate synthase and reduced folate. It inhibits synthesis of thymidylate which is in turn responsible for DNA synthesis and function.
- FUTP interferes with RNA processing and translation.
- FdUTP directly incorporates into DNA inhibiting DNA function.
Purine Antagonists
6-Thiopurines
2 agents are commonly used:
1. 6-Mercaptopurine
- Prodrug –different metabolites 6-thioinosinic acid.
- Both monophosphate and triphosphate forms produce effect, interfere with purine synthesis, ultimately DNA, RNA synthesis is affected.
- Inactivated by xanthine oxidase into 6-thiouric acid–
- Use –ALL
When used in blood cancers (leukemia) in which rapid cell turn over occurs, leading to increased uric acid and allopurinol is given, which is xanthine oxidase inhibitor, toxicity may be seen. 50-70% dose reduction is done.
2. 6-Thioguanine
- Has no drug interaction with allopurinol, is metabolized by TPMT (thiopurine methyltransferase). Some patients are genetically deficient in this enzyme, so toxicity may be seen.
Antibiotics
Anthracyclines:
- Produced by Streptomyces peucetius var caesius
Mechanism of Action
- Cause Cross linking of DNA strands
- Cause DNA breaks
- Inhibit Topoisomerase II, when DNA has to undergo replication it exists in supercoiled form, for the purpose of uncoiling certain breaks in DNA strand are made, which are then resealed. Topoisomerase II is responsible for breaks in double stranded DNA, thus no brakes are produced
- Change in membrane fluidity & ion transport, disrupting cellular functions
- Produce oxygen free radicals – cardiotoxicity
Pharmacokinetics – I/V
Toxicity
– Myelosuppression
– Mucositis
– Cardiotoxicity
I. acute –first 2,3 days in form of arrhythmias, changes in ECG, myocarditis, pericarditis
II. chronic –occurs late as dilated cardiomyopathy, cardiac failure
For prevention, patient is administered iron chelating agents. Dexrazoxane used because formation of free radicals is iron dependent, thus no iron is available.
Radiation recall reaction
If patient is already undergoing radiotherapy leads to redness, erythema, acne.
Uses
1. Cancer – breast, endometrium, ovary, testicle, thyroid, stomach, liver,lung, bladder, head & neck, soft tissue sarcoma
2. Pediatric cancers – neuroblastoma, Ewing’s sarcoma
3. Hematological cancers – ALL / AML / CML / M. myeloma / lymphoma
Mitomycin
- Antitumor antibiotic, when given, in cells converted into compounds which acts like alkylating agents.
- Hypoxic tumor stem cells –favourable areas for reduction of mitomycin
- Drug of choice with radiation therapy to kill hypoxic stem cells
Uses
- Squamous cell Carcinoma – cervix / anus
- Breast / Gastric / Pancreatic
- Administered intravasically for superficial bladder Cancer
Bleomycin
Antitumor antibiotic, small peptide having 2 binding sites:
- DNA
- Iron
Mechanism of Action – DNA-bleomycin-Fe complex is formed which is responsible for breaks
Uses – skin, cervix, vulva, head/neck, germ cell, Lymphomas
Toxicity – Pulmonary, cough, dyspnea.
On examination, inspiratory crackles are heard.
On X ray chest, infiltrates are seen.
 howMed Know Yourself
howMed Know Yourself