Hypoparathyroidism:
In hypoparathyroidism, calcium reabsorption from the bones is depressed. Metabolic changes include hypocalcemia (6-7 mg/dl), hyperphosphatemia (may be double) and hypocalciuria. Causes include:
| Contents |
| Hypoparathyroidism |
| Hyperparathyroidism |
| Primary hyperparathyroidism |
| Secondary hyperparathyroidism |
| Rickets |
| Osteomalacia |
| Osteoporosis |
| Osteopetrosis |
- Removal of parathyroid
- Autoimmune disease
- Deficiency of PTH receptors on target cells (in which case the PTH levels remain normal i.e. pseudohypoparathyroidism)
The bones remain strong because decreased osteocytic resorption of exchangeable Ca++ inactivates the osteoclasts. Hypocalcemic tetany is observed which may be localized or generalized. This is manifested by carpopedal spasm, laryngismus stridulus and obstetrician hand and latent tetany, which involves Trousseau’s sign (spasm of hand and forearm muscles) and Chvostek’s sign (spasm of facial muscles).
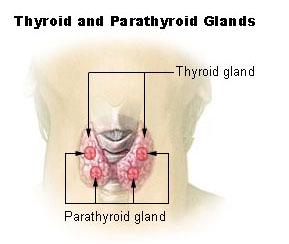
Parathyroidectomy and its Effects:
Inadvertent parathyroidectomy occurs in humans during thyroid surgery due to which a steady decline in the plasma Ca++ levels is observed. The neuromuscular hyperexcitability appears. Hypocalcemic tetany might also develop to which laryngeal muscles are especially sensitive. The plasma phosphate levels usually rise and plasma calcium levels fall.
Treatment:
Treatment involves administration of extremely large quantities of vitamin D, to as high as 100,000 units per day, along with intake of 1 to 2 grams of calcium. Administration of 1,25-dihydroxycholecalciferol instead of non activated form of vitamin D is also used.
Diseases of Parathyroid Excess:
Mutations in calcium receptor, CaR:
Mutations in calcium receptor might cause familial benign hypocalciuric hypercalcemia. Neonatal severe primary hyperparathyroidism is also possible. Familial hypercalciuric hypocalcemia is also possible.
Hypercalcemia of Malignancy:
Hypercalcemia is also a common metabolic complication of cancer.
Local osteolytic hypercalcemia involves bone metastasis that produces the hypercalcemia by eroding bone.
Humoral hypercalcemia of malignancy involves elevated levels of PTHrP or cancers of breast, kidney, ovary and skin.
Hyperparathyroidism:
a. Primary Hyperparathyroidism
Primary hyperparathyroidism is caused by excess PTH secretion. PTH-secreting adenomas are asymptomatic. It occurs more frequently in women. Extreme osteoclastic activity is observed in the bones. Osteoblastic activity also increases in the bones. Calcium ion concentration is elevated in the extracellular fluid, while concentration of phosphate ions is usually depressed. Serum alkaline phosphate levels are usually high.
Radiographs of the bones show extensive decalcification. Other observations include:
- Multiple fractures
- Osteitis fibrosa cystica-bones are eaten away in severe hyperparathyroidism i.e. slow, extensive decalcification with ‘punched out cystic areas’
- Parathyroid poisoning and metastatic calcification
- Kidney stones- due to crystals of calcium phosphate
Effects of Hypercalcemia in Hyperparathyroidism
Hyercalcemia in hyperparathyroidism leads to plasma calcium levels greater than 12 mg/dl which causes:
- Depression of central and peripheral nervous system.
- Muscle weakness and constipation
- Abdominal pain
- Peptic ulcer
- Lack of apetite
- Depressed relaxation of heart during diastole.
- Sluggish reflexes
- Anorexia
- Reduced ST segment and QT interval.
If plasma calcium levels rises above 15 mg/dl, the symptoms become severe. Plasma calcium levels greater than 17 mg/dl are lethal causing parathyroid poisoning.
Parathyroid Poisoning and Metastatic Calcification:
Very high plasma calcium levels above 17 mg/dl and high plasma phosphate levels causes deposition of calcium phosphate crystals in:
- Alveoli and Tubules of kidneys
- Thyroid gland
- Acid producing areas of stomach
- Walls of arteries
- Death in a few days
In relatively mild hyperparathyroidism increased calcium levels cause renal stone formation.
b. Secondary Hyperparathyroidism
Secondary hyperparathyroidism might occur:
- As a compensation for hypocalcemia
- In chronic renal disease- due to the fact that kidneys are unable to produce sufficient amounts of active form of vitamin D (1,25- dihydroxycholecalciferol)
- In rickets- due to vitamin D deficiency
Rickets:
Rickets is the vitamin D deficiency which involves decreased calcium and phosphate levels in the body. It occurs mainly in the children and may be due to:
- Inadequate intake through diet
- Inadequate exposure to sunlight or in smoggy cities.
An increase in osteoblastic activity is observed which involves increased osteoid, which is not calcified. Inadequate mineralization of epiphyseal plates in growing bones occurs due to inadequate amounts of calcium and phosphates. Tetany almost never develops.
Manifestations:
Manifestations involve:
- collapse of chest wall
- Rachitic rosary
- kyphosis
- lordosis
- scoliosis
- Harrison’s sulcus (groove in ribs due to inward pulling of diaphragm)
- bowing of weight bearing bones e.g. legs
- dental defects.
Osteomalacia:
Osteomalacia or adult rickets is severe dietary deficiency of vitamin D or calcium in adults. It seldom occurs.
Causes:
- Steatorrhoea
- Chronic renal disease (Renal rickets)
- Dialysis induced bone disease
Defective calcification of bones occurs.
Features:
Features include:
- Vague pain
- Tenderness in bones and muscles
The person is resistant to vitamin D treatment.
Osteoporosis
Osteoclastic activity greater than osteoblastic activity with the loss of bone matrix is known as osteoporosis. Fractures are common and include:
- Colle’s fracture (forearm)
- Vertebral body
- Hip kyphosis
- “Widow’s hump”
Causes:
Causes include:
- Lack of physical stress/immobilization
- Lack of vitamin C
- Decreased estrogens (postmenopausal)
- “Involutional osteoporosis”
- Old age
- Cushing syndrome
Osteopetrosis:
Osteopetrosis occurs due to defective osteoclasts, due to which the osteoblasts operate unopposed and result in increased bone density. Neurological defects occur due to narrowing of foramina and hematological abnormalities occur due to crowded marrow cavities.
 howMed Know Yourself
howMed Know Yourself