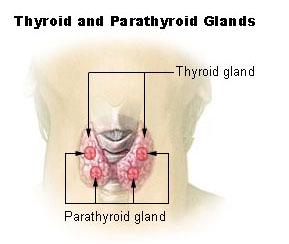
 Hyperparathyroidism
Hyperparathyroidism
Hyperparathyroidism may be primary or secondary.
1. Primary hyperparathyroidism
a. Sporadic
Causes
· Solitary adenoma (commonest)
· Cheif cell hyperplasia
· Carcinoma
b. Familial
· MEN = multuple endocrine neoplasia type-I Werlmer’s syndrome
· Autosomal dominant = as with inactivating germ line mutation of MEN-1 TSG on Ch-II
Clinical
- Hyper PTH > 80%
- Benign pituitary adenomas (functioing/non functioning)
- Parcreatoco-duodenal neuroendocine tumors (Beingn / malignant)(gastrinoma, insulinoma, insulinoma, glucagonoma, vipoma & other peptide hormones
MEN-2
· Occur in MEN-2A & renal in MEN-2B
Familial isolated hyper PTH
· Increased risk of PT carcinoma
2. Secondary hyper PTH
Due to chronic renal failure,
D Decreased calcitriol leads to decreased calcium & PO4 retention causing proliferation of PT cells and increase in gland parendepmal mass
3. Tertiary hyper PTH
Renal osteodystrophy, following renal transplantation, development of autonomous hyper function of PT tissue & increased calcemia
4. Parathyroid Ca
5. Persistant / recurrent hyper PTH
Ca occuring more than 1 yr after creative parathyroidectomy
Causes
· Missed pathology at 1st surgical procedure
· Graft dependent recuence
· Parathyromatosis disseminated nodules of PT tissue within soft tissue of neck & suspicious mediastenemia caused by abnormal PT tissue at initial surgery. (reoperative PT surgery,risk of recurrent laugeal nerve injury & postopCa)
Causes of hypoparathyroidism
1. Primary hypoparathyroidism
PTH deficiency
Causes
1. Surgical damage to glands (common)
- During thyroidectomy
- Radical neck dissection
- Resection of PT gland in PT hyperplasia
2. Radiation therapy to neck
3. Damage from
- Infection
- Metastatic tumor
- Infiltration by granuloma (TB, sarcoidosis)
- Heavy metals (Wilsons, hemocheomatosis, transfusion hemosiderosis)
4. Hormone – Resistant (inherited) (Pseudohypoparathyroidism = PHP)
End organ resistance to PTH, plasma levels of which are hight in response to hypocalcemia
PHP = type (1a & 1b)
· Inability of PTH to generate an increase in urinary (AMP, PHP = type-II)
PHP type-II
· Inability of PTH to generate an increase in phosphaturic response
Idopathic
Dysembryogenesis (Di-George’s syndrome)
Appears as familial disorder, may have autoimmune basis presents at puberty where it is associated with mucoutaneous candidiasis due to immune def & other endocrine disorders.
Magnesium Deficiency
· Serum magnesium < 0.4 mmol/L)
· Suppresion of PTH secretion becoming unresponsive to calcium therapy unless patient becomes magnesium-replete.
 howMed Know Yourself
howMed Know Yourself