It is the most common example. The proliferative activity of endometrium is controlled by increased estrogen, which is then stopped by increase in progesterone levels. If there is imbalance between estrogen and progesterone secretion, the level of estrogen remains high, causing pathological hyperplasia of the endometrial glands, which may be benign or malignant.
Conditions leading to endometrial hyperplasia are:
- Polycystic ovarian disease
- Granulosa cell tumors
- Prolonged administration of estrogenic substances such as estrogen replacement therapy.
- Menupause
- Cortical stromal hyperplasia
Morphology
Endometrial hyperplasia is divided into:
a. Simple or Cystic hyperplasia
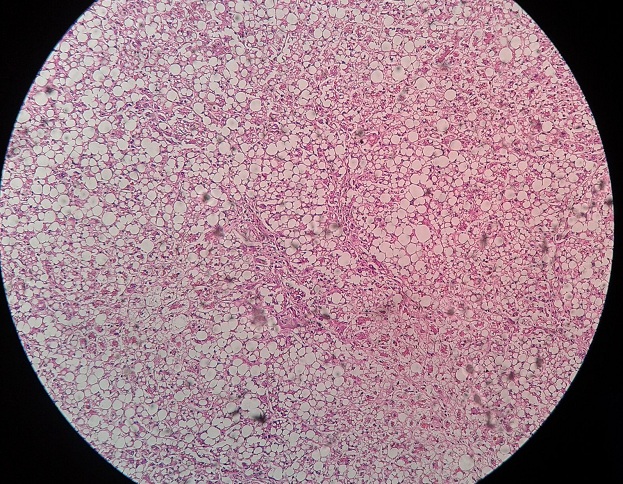
There will be change in architecture of gland producing cystic dilatations and back to back lined glands. The epithelial growth pattern will be similar to proliferative endometrium i.e. multilayered glands can be seen, also known as stratification of glandular epithelium. Mitosis is not very apparent and stroma between the glands becomes dense.
b. Complex Hyperplasia
It is also known as adenomatous hyperplasia without atypia. There will be increase in number and size of glands. The glands become irregular shaped with finger like projections. The epithelial lining becomes more stratified but without atypical changes.
c. High Grade Hyperplasia
Also known as atypical or adenomatous hyperplasia with atypia. There is glandular crowding. The glands become more irregular in shape and epithelial lining also becomes irregular with stratifications. Cellular atypia with cytomegaly, hyperchromatism, prominent nucleoli, altered nuclear to cytoplasmic ratio, mitotic figures are common. 23% patients with high grade hyperplasia develop adenocarcinoma.
 howMed Know Yourself
howMed Know Yourself