Tuberculosis is a chronic disease caused by mycobacteria, which are acid fast bacilli, once stained by basic dyes, cannot be decolourized by alcohol. Acid fast character is due to the presence of mycolic acids in cell wall. It gives integrity to cell wall and makes it resistant against antibiotics. Mycobacteria are of two types:
a. Typical Mycobacteria
- M tuberculosis
- M bovis
- M leprae
b. Atypical Mycobacteria
These bacteria are less pathogenic but more resistant to common anti-tuberculosis drugs.
- M kansasii
- M marinum
- M scrofulaceum
- M avium complex
- M chelonae
- M fortuitum
- M ulcerans
Treatment of Tuberculosis
There are three main principles of treatment of tuberculosis:
- Rest
- Prolonged chemotherapy
- Follow up
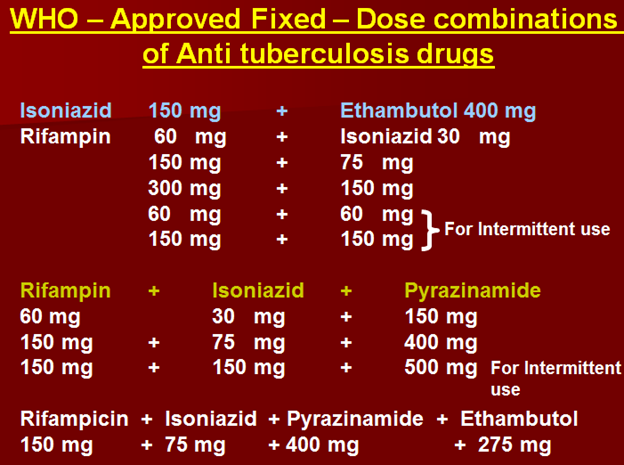
In treatment of tuberculosis, we give a combination of drugs. Treatment is started with two or more drugs. The reason for combination is that if bacteria become resistant against one drug, others can still act. Treatment is started with three or four drugs and continued with two drugs.
There are two main difficulties:
- Patient compliance –as drugs have to be taken for prolonged duration
- Chances of toxicity
The main drugs are:
First line drugs (mainly used, treatment is started with these)
- Isoniazid
- Rifampicin
- Pyrazinamide
- Ethambutol
- Streptomycin
Second line drugs (only in cases resistant to 1st line)
- Amikacin, thiacetazone
- Para amino salicylate
- Ethionamide
- Ciprofloxacin/ofloxacin
- Rifabutin
- Clarithromycin
- Cycloserine
- Capreomycin
Drugs for atypical mycobacteria
- Erythromycin
- Clarithromycin
- Azithromycin
- Rifampicin
- Quinolones
- Rifabutin
Isoniazid
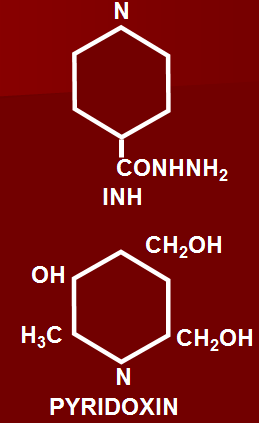
Chemically drug is hydrazide of isonicotinic acid.
Anti-bacterial Spectrum:
Has a narrow spectrum. Effective only against mycobacterium tuberculosis. Also has some effects against atypical mycobacteria.
Mechanism of action of isoniazid
Drug enters the bacterial cells by active transport mechanism and is bactericidal for rapidly dividing cells and bacteriostatic for resting or dormant bacterial cells.
Drug is a prodrug and in bacterial cells is converted to active compound by enzyme catalase peroxidase. This active form acts by:
- Inhibition of mycolic acid synthetase responsible for synthesis of mycolic acid in cell wall, resulting in damage to cell wall and increase in permeability, leading to entry of water and death of bacterial cell.
- Inhibition of nucleic acid synthesis in bacteria
- Inhibition of lipid synthesis
- Inhibition of glycolysis
Mechanism of resistance
Develops by various mechanisms:
- Mutation/deletion of catalase peroxidase (katg) responsible for converting the drug to active form
- Mutations in various transporters in bacterial cell
- Mutation of acyl carrier proteins
- Over expression of NADH dependent acyl carrier protein reductase (INHA) enzyme
Pharmacokinetics
Well absorbed after oral administration. Peak plasma concentration occurs after 2-4 hours. After absorption drug is easily distributed to all body compartments.
It can penetrate macrophages, caseous material, can easily penetrate into CNS. It distributes well in all body compartments including CNS and caseous material in lungs.
Metabolized by acetylation. There are genetically two kinds of people:
- Slow acetylators –half life in these is 4 hours
- Fast/rapid acetylators –half life in these is 1 hour
Most of the drug and metabolites are excreted in urine.
Uses of isoniazid
Reserved for the treatment of tuberculosis, used in various forms of tuberculosis.
- Active tuberculosis
- Tuberculin positive converters of close contact with active cases (prophylactically)
- Tuberculin positive cases on immuno suppressive or antineoplastic chemotherapy (prophylactically)
Dose: 300mg/day
Advantages of isoniazid
- Highly selective against mycobacteria
- Bactericidal action
- Cost- effective/easily available
- Orally administered
- Well absorbed
- Widely distributed in body tissues/ fluids
- Enters macrophages
- Penetrates caseous material
- Crosses blood brain barrier
- Once daily administration
- Well tolerated
Adverse effects – isoniazid
- Peripheral neuropathy
Most important adverse effect. Manifested in the form of:
- Numbness
- Change in sensations of touch, temperature, pain
- May affect motor functions
- Weakness of muscles
- Mainly affects sensations
Occurs mainly due to decreased/deficiency of vitamin B6 or pyridoxine.
The main thing is that it interferes with the metabolism of pyridoxine. It also causes increased excretion of this vitamin.
Person routinely taking isoniazid is given tablets of pyridoxine in dose of 10 mg daily to avoid peripheral neuropathy.
- Hepatotoxicity
Occurs especially in elderly and patients who are alcoholic.
- Hypersensitivity reactions
- Skin rashes
- Articaria
- Maculopapular rash
- Leukopoenia
- Thrombocytopenia
- Hemolytic anemia esp. in patients with G6PD deficiency
- Hematological reactions
- Vasculitis
Rare but may occur especially when given parentally.
- Arthralagia
In joints pain especially in knee, elbow, wrist and joint of fingers.
- Mental disturbances (CNS toxicity)
- Headache
- drowsiness
- GIT upsets
- Methaemoglobinaemia
- Incordination
- SLE like syndrome –although rare but may occur
Drug Interactions
- May cause inhibition of microsomal enzymes especially those of hydroxylation so increased levels are observed of:
- Phenytoin
- Carbamazepines (anti-epileptics)
- Also cause CNS stimulation when given in combination with monoamine inhibitors.
Rifampicin
Very important drug in the treatment of tuberculosis, belonging to the rifamycin group of antibiotics. It is obtained from Streptomyces species. Mainly rifamycin B is modified to obtain rifampicin.
Mechanism of action
Drug mainly acts by inhibiting DNA dependent RNA polymerase enzyme in bacteria. This enzyme is mainly responsible for formation of mRNA. When inhibited no or less formation of mRNA occurs, resulting in decreased formation of proteins. The important fact is that this bactericidal action differs from other drugs which inhibit protein synthesis, as most of them are bacteriostatic drugs. Here it is bactericidal, as it acts on transcription level.
Resistance
Mainly occurs:
- Due to mutation in DNA dependent RNA polymerase enzyme, which has less affinity for drug
- There is decreased entry of drug into bacteria.
Spectrum Of Activity – Rifampicin
Has wide antibacterial spectrum. In addition to mycobacteria affects various gram positive and negative bacteria:
- M. tuberculosis
- M. leprae
- Atypical mycobacteria
- Gram negative microorganism e.g. E.coli, pseudomonas, Proteus, Klebsiella, Brucella, H.Influenzae, N.meningitidis
- Staphylocci
- Meningococci
- Legionella
- Chlamydia
- Anti viral activity (pox virus)
Pharmacokinetics
Well absorbed after oral administration. Peak plasma concentration occurs after 2 hours. Drug is easily distributed to all body compartments including CNS.
It is mainly metabolized in liver by deacetylation, drug also undergoes enterohepatic circulation.
Most of the drug is excreted in feces through bile.
Half life is about 3 to 5 hours. On prolonged use it is decreased even up to 2 hours as is enzyme inducer.
Therapeutic uses of Rifampicin
- Tuberculosis (in combination with other tuberculosis drugs)
- Leprosy
- Atypical mycobacterial infections
- Chemoprophylaxis for meningococcal disease and meningitis due to H. influenzae
- Staph. endocarditis or osteomyelitis
- Eradication of staph. nasal carrier state in chronic furunculosis
- Brucellosis –in combination with doxycycline
- Legionnaire’s disease –in combination with ciprofloxacin and quinolones
Dose: 450 – 600mg/d or 10-20mg/kg
Adverse effects – rifampicin
- Hepatotoxicity –as metabolized in liver and excreted in bile
- Thrombocytopenia
- Cutaneous reactions -articaria
- Discoloration of secretions especially orange colour of urine, sputum, various body secretions. It is harmless, actually indicates that patient is taking the medicine.
On intermittent dosing –immediately after administration of drug due to immunity and immunological basis:
- Flu – like syndrome –chills, fever, malaise, myalgia, joint pain
- Acute hemolytic anemia
- Acute renal failure
Drug Interactions
Drug is enzyme inducer and can increase the metabolism of various drugs.
Rifabutin
Differs from rifampicin in that although mechanism of action and chemistry is same as rifampicin, but differs in:
- Longer half life of 36 hrs.
- Less drug interactions
- In adverse effects differs in that when given in high doses, in combination with other drugs, enzyme inhibition may cause toxicity especially reversible uveitis.
Mainly used in resistant cases of tuberculosis in combination with other drugs, can also be used in prophylaxis of tuberculosis in close contacts.
Dose: 300mg OD
When given with enzyme inhibitors like HIV Protease Inhibitors including Indinavir & Ritonavir, and non nucleoside reverse transcriptase inhibitors, dose is reduced to half (150 mg).
Rifapentin
- Half life 13 hrs.
- Potent enzyme inducer
- Active metabolite is desacetyl rifapentin
Dose: 600 mg once or twice weekly
Pyrazinamide
Derivative of nicotinamide.
Mechanism of action
Drug is very effective against mycobacteria, residing in cells and dormant. It is more active in acidic medium of cells.
More effective inside cell (acidic medium), it is a pro drug converted into cell to active metabolite pyrazinoic acid by enzyme pyrazinamidase.
Bactericidal –Kill persisters
Pharmacokinetics
Well absorbed after oral administration. Distributes to all body compartments well. It crosses blood brain barrier and attains a high concentration in CSF.
Drug is always used in combination with other drugs for tuberculosis and meningitis.
It is metabolized in liver and half life is 9 hours.
Uses
- Treatment of tuberculosis in combination with other drugs specifically mycobacterium tuberculosis.
- Has little activity against mycobacterium bovis.
Dose:20-30mg/kg or 1.5 -2.5g/day upto 3gm
Adverse effects
- Arthralgia –active metabolite pyrazinoic acid is responsible for hyperuricemia as decreases the secretion of uric acid.
- Hepatitis –in high doses
- GIT upsets
- Hemolytic anemia
- Allergy
- Dysuria
- Sideroplastic anaemia
Ethambutol
- L isomer – toxic
- D isomer – active (mainly used in therapeutics)
- b isomer – no antibacterial activity
Mechanism of Action
Drug is rapidly uptaken by cells. Resistance develops when decreased uptake of drug occurs by bacterial cells. It:
- Inhibits incorporation of mycolic acid in bacterial cell wall
- Inhibits RNA synthesis
- Inhibits mycobacterial arabinoglycan synthesis in cell wall
Pharmacokinetics
- Well absorbed after oral administration. Peak plasma concentration occurs after 2-4 hours.
- Drug attains high concentration in lungs.
- It also enters CSF when meninges are inflamed, thus can be used for tuberculosis meningitis.
- Two thirds of the drug are excreted unchanged in urine, rest is metabolized in the liver.
- Half life is about 4 hours.
Uses
Mainly used for treatment of tuberculosis in combination with other drugs.
Adverse Effects
Mainly when given in high doses:
1. Ocular effects
- Retrobulbar neuritis
- Red green colour blindness
Although incidence is rare (2%) but can lead to blindness if continued.
2. Increase plasma uric acid
3. GIT effects
4. CNS –drowsiness, confusion
Dose: 15mg/kg to 25mg/kg
Streptomycin
Aminoglycoside used in combination with other anti-tuberculosis drugs.
Second line drugs
In second line drugs, Amikacin belongs to aminoglycosides. Thiacetazone is a toxic drug having low therapeutic index, which is very cost-effective. It is used as a second line drug in treatment of tuberculosis. Half life is 13 hours. Main adverse effects are:
- GIT upsets
- CNS problems
- Arthritis
- Blood dyscrasias –leukopoenia, hemolytic anemia
Para amino Salicylate (PAS)
Chemically it resembles PABA (sulfonamides).
Mechanism of action is same as sulfonamides.
Acts by inhibiting synthesis of folic acid, folic acid synthetase in inhibited. Drug is bacteriostatic.
Pharmacokinetics
Well absorbed after oral administration. Always given with food. Drug distributes in all body compartments except CSF. It cannot cross BBB.
Metabolized by acetylation. Half life is one hour.
Drug is mainly used as a second line drug in treatment of tuberculosis.
Dose: High 10-20 grams
Adverse effects
1. Drug mainly causes GIT upsets
2. Allergic reactions –articaria
3. Blood dyscrasias
- Leukopoenia
- Thrombocytopenia
- Hemolytic anemia in G6PD deficiency
4. Hypothyroidism when used for prolonged period.
Ethionamide
Chemically resembles isoniazid.
Mechanism of action
Mechanism of action is same, it interferes with synthesis of cell wall.
Half life is about 2-4 hours. It is a very toxic drug and is mainly reserved for resistant cases of tuberculosis.
Adverse effects
- GIT problems
- Allergic reactions
- Blood dyscrasias
Dose is 250 mg twice daily, which may be increased to 1 g daily.
Ciprofloxacin
Clarithromycin
Cycloserine
Obtained from Streptomyces. Chemically drug resembles d-alanine (cell wall synthesis, peptidoglycan synthesis)
Mechanism of action
Same as that of penicillins. Interferes with synthesis of peptidoglycan.
When given orally, well absorbed. About 35% of drug is metabolized, rest is excreted unchanged in urine.
Adverse effects
Main are on:
- CNS –neurotoxic effect, as drug crosses BBB.
- Headache
- Drowsiness
- Dizziness
- Convulsions
Dose 15-20 mg/kg body weight.
Capreomycin
Resembles aminoglycosides.
Mechanism of action –same as that of aminoglycosides
Adverse effects –same. May cause:
- Ototoxicity
- Nephrotoxicity –main effect
Steroids in Tuberculosis
- Massive pleural effusion
- Pericardial effusion
- Tuberculous meningitis
- Miliary tuberculosis with involvement of adrenal cortex
Regimens Of Antituberculosis Drugs
There are two main phases:
- Start with 3 or 4 drugs, called induction phase
- Continued with 2 or more drugs known as continuation phase.
New Cases
Patients who have not received treatment for T.B previously
Patients who have taken the treatment for less than 4 weeks
Initial Intensive Phase -For 02 months
- Isoniazid
- Rifampicin
- Pyrazinamide
- Ethambutol
Continuation Phase -For 06 months
- Isoniazid
- Ethambutol
In continuation phase, rifampicin is not used with isoniazid, because patient may develop resistance to isoniazid, making the therapy monotherapy. Thus resistance against rifampicin may also develop.
In Western countries, Rifampicin is preferred in continuation phase, with which duration of treatment is reduced to 7 months.
Re- Treatment Cases
In cases of relapse, after 1 to 2 months if symptoms disappear and patient stops taking drugs, there is re-emergence of tuberculosis, which is difficult to treat, resulting in treatment failure.
Now the treatment is started with five drugs.
Intensive Phase -For three months
- Rifampicin
- Isoniazid
- Pyrazinamide
- Ethambutol
- Streptomycin -For first two months
Continuation Phase -For five months
- Rifampicin
- Isoniazid
- Ethambutol
Intermittent Regimens –given twice weekly
- Streptomycin 1g
- Isoniazid 15 mg/kg
- Ethambutol 50 mg/kg
Multiple Drug Resistant Tuberculosis (MDR-T.B)
If patient is resistant to INH and rifampicin after about 5 months treatment, still acute tuberculosis bacilli is present in sputum, the patient is labeled multiple drug resistant.
Treatment is the use of second line drugs.
DOT (Directly observed therapy)
Patient takes medicine in clinic or undergoes supervised treatment in hospital. Patient may be called twice or thrice weekly and given anti–tuberculosis drug in front of the doctor or medical personelles. This is because the main problem is compliance of the patient.
 howMed Know Yourself
howMed Know Yourself