These drugs are used for:
1. Peptic ulcers (gastric or duodenal)
2. Gastro esophageal reflux disease
3. Hyper secretory conditions –Zollinger Ellison syndrome
Underlying Causes of Ulcers
- Helicobacter pylori a gram negative bacillus is a major cause of duodenal ulcer.
- Imbalance between acid/pepsin secretion
- Decreased secretion and action of mucous/bicarbonates.
Histamine, acetylcholine and gastrin provide stimulus for release. Balance is maintained by opposing effects of mucous, bicarbonates, prostaglandins and superficial layer of epithelial cells. Any disturbance may lead to development of ulcers.
Drugs can alter the balance towards prevention or healing of Ulcer
- Reduction of acid secretion
- Neutralization of secreted acid
- Eradication of helicobacter pylori
- Enhanced mucosal resistance
The Control of Gastric Acid Secretion
Gastric acid (HCl) is produced by parietal cells in the stomach and its secretion is regulated by three pathways.
- Parasympathetic stimulation occurs via the vagus nerve, the preganglionic fibres of which synapse at ganglia where muscarinic M1 receptors play an important role in neurotransmission.
- Gastrin is released from G cells in the antrum of the stomach
- There is a local release of histamine from enterochromaffin-like (ECL) cells.
Stimulation of prostanoid receptors PGE2, PGI2 on superficial epithelial cells inhibits HCl secretion.
Imbalance leads to development of peptic ulcer.
H2 receptor antagonists are required in high dose in hypersecretory conditions, so no more used. Large amount of antacids is required.
Drugs Used In Peptic Ulcer
Drugs that Reduce Acid/Pepsin Activity
H2-Receptor Blockers
- Cimetidine,
- Ranitidine,
- Famotidine,
- Nizatidine
Proton Pump Inhibitors (Benzimidazole Derivatives)
- Omeprazole,
- Lansoprazole,
- Rabeprazole,
- pantoprazole,
- Esmoprazole (S isomer omeprazole)
Anti Muscarinics (M1 Selective) (control acid secretion)
- Pirenzepine,
- Telenzepine
Gastric Antacids
Systemic
Sodium bicarbonate
Non Systemic
a. Physicochemically acting
- Aluminium hydroxide,
- Al phosphate
- Magnesium trisilicate,
- Magaldrate
b. Chemically acting
- Magnesium hydroxide,
- Ca carbonate (non ulcer dyspepsia)
Drugs that Increase Mucosal Resistance
Sulfated Sucrose Derivative
Sucralfate
Colloidal bismuth compounds
- dicitrato tripotassium bismuthate,
- bismuth subcitrate
Prostaglandin derivative
- misoprostol,
- enprostil,
- rioprostil
Drugs used for the Eradication of Helicobacter Pylori (Antibiotics)
- Metronidazole
- Clarithromycin
- Amoxicillin
- Tetracycline
Proton Pump Inhibitors
Omeprazole
Mucosal Surface Protectors
Bismuth salts (better options are available)
Antacids
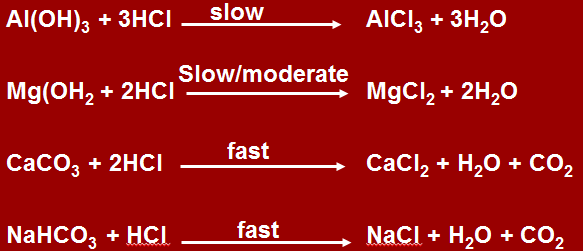
Chemical Composition
AlCl3 is demulcent, forms coating over ulcerated mucosa. Problem is that it has astringent property leading to constipation.
MgCl3 has weak chemical action, there are chances of toxicity with Mg. It is prescribed in combination with Al to increase buffering time.
CaCl2 has complete absorption, neutralization can take place repeatedly, so not preferred because of toxicity.
CO2 causes belching.
Systemic acting are not given, as increase Na load may lead to cardiac problems.
If heart burn occurs, and milk is given along with systemic antacids (soda bicarbonate containing, Ca containing or in renal compromised) can lead to milk alkali syndrome, leading to hypercalcemia and toxicity.
If peptic acid is confirmed, systemic acting are not given because of:
- Belching
- Milk alkali syndrome
- Acid rebound –systemic antacids neutralize gastric pH when taken continuously, poor neutralization reflex gastric secretion, even when stop taking, gastrin is in excess.
H2 Receptor Antagonists
- Competitively inhibit histamine actions at all H2 receptors
- Lowers the basal, food stimulated & nocturnal secretions of gastric acid as histamine release is maximum at night.
Now proton pump inhibitors are the main stay.
- Rapidly absorbed after oral administration, oral preparations are preferred, I/V preparation is available as well. Given I/V in stress and gastric bleeding.
- under go first pass hepatic metabolism
- Bioavailability 50%
- Nizatidine has negligible first pass metabolism. Cimetidine undergoes 1st pass metabolism.
- Therapeutic levels achieved rapidly after I/V dosing
- Duration of action depends on dose given
- Excretion by kidneys
- Important to reduce dose in patient with decreased creatinine clearance.
Cimetidine is imidazole derivative, nocturnal dose of 800 mg quite sufficient for 24 hour acid secretion.
Ranitidine (zantax) has similar actions, 300 mg nocturnal dose while Famotidine has triazole ring (400 mg). 5 times more potent, mainly used.
Nazitidine has 20 mg dose, not used for nocturnal treatment, used for symptomatic treatment, for short term. NSAIDs are used as these are not cost effective.
| Cimetidine | Ranitidine |
| 5 times potent | |
| Undergoes 1st pass metabolism | Does not undergo (only 10%) |
| Action mainly GIT | |
| I/V within 4-5 hours effect | 6-8 hours levels up to 12 hours remain after I/V admin |
| Avoid in young adults having adrenergic effects. | |
| Excretion through kidneys, one has to be careful as renal impairment might occur. |
Adverse Reactions
Well tolerated by most patients, occur in less than 3%
Minor:
a. Diarrhea, abdominal pain
b. constipation
c. head ache,
d. Drowsiness,
e. Fatigue,
f. Muscular pain,
CNS:
a. Confusion,
b. delirium,
c. Hallucination –not seen with oral administration at therapeutic doses
d. slurred speech,
e. headache in elderly or /IV route
Long Term Use of Cimetidine at High Doses
Rare but chances of certain adrenergic side effects:
- decreases testosterone binding to the androgens receptors (infertility/impotency chances)
- inhibits cytochrome that hydroxylates estradiol & inhibit degradation of estradiol –galactorrhea, gynecomastia
- blood dyscrasias thrombocytopenia
- hypotension/ bradycardia I/V esp. in patients having cardiac problems
Drug Interactions
Mainly with cimetidine, Inhibit CYP1A2, CYP2C9 CYP2D6
- Tolerance to acid suppressing effect, may develop within 3 days –one reason why not commonly used
- Secondary hyper gastrin emipa
Rebound increase in acid secretion even after the drug is stopped (also by systemic antacids)
Therapeutic Uses
- To promote healing of gastric/duodenal ulcers
- To treat uncomplicated GERD
- To prevent occurrence of stress ulcer
- Cases of GERD in pregnancy with ranitidine
Anti muscarinic drugs
Although decrease basal secretion, do not increase pH to sufficient levels, although H2 blockers are used, which reduce secretions already.
Adverse effects include:
Abdominal discomfort, spasms, pain
Parenzepine and Olenzapine are M1 drugs helpful in some patients.
Because of M2 blockage, atropine is NOT USED, may cause tachycardia, dry mouth and urinary retention.
May promote secretion of mucous bicarbonates having limited role
Proton Pump Inhibitors
- All are substituted benzimidazoles
- Prodrugs, lipophilic weak bases
- Racemic mixtures R and S isomers,
- Inhibit the final common step in gastric acid secretion
- All types available as oral formulations, enteric coated
- Esmoprazole, pantoprazole also as I/V formulations
Lanosprazole is given orally, can disintegrate in mouth, is water soluble given in ITC. Can be given dissolved in water as well, or enteral route or by oral syringe. When enteric coated tablets are given, at alkaline pH, disintegrate and drug is released, all stimuli of gastric acid secretion are inhibited. Very effective as H K ATPase is the final step, if inhibited secretion becomes zero.
Mechanism of Action
- at acidic pH it secretes into a reactive thiophilic sulfphenamide cation.
- reacts covalently with SH GP of the H+ K+ – ATPase enzyme,i nactivates it irreversibly
- Gets concentrated in the acidic pH of the parietal cell canaliculi
- HCl secretion resumes only when new H+ K+ ATPase molecules are synthesized
Pharmacokinetics
- Administered empty stomach 01 hr before break fast.
- Short serum half life 1.5 hrs, but acid inhibition last for 24 hours
- Rapid first pass hepatic metabolism
- I/V prep are preferred as continuous infusion to provide max. inhibition initially.
Clinical Uses
- Non erosive & erosive reflux disease (GERD)
- Symptomatic GERD -first line therapy
- Duodenal ulcer 90% healed 4 wks, Gastric ulcer 6-8 wks 90% as mucosal damage occurs
- NSAIDS associated ulcers.
- Prevention of rebleeding from peptic ulcer.
- Prevention of stress related mucosal bleeding .
Omeprazole is administered by nasogastric tube
FDA approved oral immediate release fluids are available.
Adverse Effects
Safe drugs,
1. GIT
- Diarrhea,
- headache,
- abdominal pain (1-5% patients)
2. With prolonged therapy, vitamin B12 levels decreased
5. Hospitalized patient may have an increased risk for clostridium difficile infection .
6. ECL hyperplasia in response to hypergastrinemia.
7. May reduce Ca absorption or inhibit osteoclast function – risk factor for those with osteoporosis
8. Increase in gastric bacterial concentration, increase risk of community acquired respiratory infection & nosocomial pneumonia among patient taking proton pump inhibitors.
Drug Interactions
Ketoconazole, Digoxin and antivirals, because of decreased acid secretion. (Atonavir actions are impaired)
Omeprazole inhibits metabolism of Diazepam and warfarin, Diazepam action is prolonged.
Combination of drugs used for the treatment of peptic ulcers due to H. Pylori infections
3 regimens are in the guidelines, depending upon lesions and compliance of patient. Combination increases buffering time, overuse may lead to side effects:
- Omeprazole 20mg twice daily before meals or lansoprazole 30 mg twice daily + metronidazole 500 mg twice daily + clarithromycin 500 mg twice daily after meals.
- 20 mg Omperazole or 30 mg lansoprazole twice daily before meals + 1 g of amoxycillin twice daily + 500 mg of clarithromycin twice daily after meals
- 240 mg of bismuth chelate 4 time daily + tetracycline 500 mg 4 time daily + metronidazole 250 mg 4 time daily. Quite cumbersome because:
- has to be taken four times daily. If not responding to first two drugs then given. It was used as detaches from intestine and cause lysis. Additionally having mucoprotective role causing increase in secretion of mucous.
- Blackening of tongue
- Patient compliance is poor
All the above regimens should be given for 10-14 days. After this a further course of omeprazole 20 mg once daily for 2 weeks or Lansoprazole 15 mg once daily for 2 weeks should be used for cases With duodenal ulcer. In patients with gastric ulcer omeprazole 40 mg And lansoprazole 30 mg should be given for further 6 weeks. H2 antagonists or sucrlfate can be given instead of proton pump inhibitors after the completion of 10-14 days regimens for H-Pylori eradication.
Prostaglandins
Prostaglandins have cytoprotective role TGE2, TGI2 by:
- Inhibiting acid secretion
- Promote healing of damaged gastric mucosa
- Increases microcirculation
- Enhances tight junctions of mucosa so that back diffusion does not occur.
Have very short half life. A number of stable prostaglandins analogs are available.
Misoprostol is given in 800 mg dose, given 3-4 times daily, effective in duodenal ulcer treatment but in initial one week treatment, induce pain themselves. Patient compliance is poor, reserved for gastroduodenal ulcers or NSAIDs induced.
Misoprostol (Cytotec ®)
Drug Class: Prostaglandin analog (synthetic)
Mechanism of Action
A methyl analog of PGE1. It is believed to stimulate mucus & bicarbonate secretion & enhance mucosal blood flow, thereby helping protect the stomach by forming a protective barrier against acid. It also binds to prostaglandin receptors on parietal cells, reducing histamine-stimulated cAMP production & causing modest inhibition of acid secretion.
Not superior to PPH and H2 antagonists.
Indications
Prevention of NSAID (including aspirin)-induced gastric ulcers in patients at high risk of complications from gastric ulcer, e.g., the elderly and patients with concomitant debilitating disease, as well as patients at high risk of developing gastric ulceration, such as patients with history of ulcer.
Contraindications:
Contraindicated, because of its abortifacient property, in women who are pregnant. Women of childbearing potential should be told that they must not be pregnant when misoprostol therapy is initiated, and that they must use an effective contraception method while taking misoprostol.
Side Effects:
Diarrhea, increased uterine contractions
Mucosal Protective Agents
Drug: Sucralfate (generic, Carafate ®)
Drug Class: Mucosal Protective Agent
Mechanism of Action:
Sucralfate is a salt of sucrose complexed to sulfated aluminum hydroxide.
Sucrose octasulphate + polyalumonium hydroxide
- When administered, required acidic pH is below 4. At less than 4, since complex, polymerization and cross linking different polymers are converted into viscous, tenacious paste that binds selectively to ulcers or erosions for up to 6 hrs. It is believed that the negatively charged sucrose sulfate binds to positively charged proteins in the base of ulcers or erosions, forming a physical barrier that restricts further caustic damage.
- Local production of epidermal factors stimulated
- Does not gets absorbed having physical action
Have to be given in high doses 4 times a day. 1g before each meal and at sleeping time. Duration of treatment is 4-6 weeks.
Have to stop other treatments as activated at acidic pH so cannot be given with H2, PPH or antacids, otherwise cannot get activated.
But protective layer is short lived given temporarily.
Indications:
Treatment of duodenal ulcer.
Pharmacokinetics:
Less than 3% of intact drug gets absorbed into the body. The remainder gets excreted in the feces.
Side Effects:
Constipation, black stool
Major drug interactions:
Don’t take with H2 blockers or antacids, which reduce the acidic environment required for activation of sucralfate.
Drug: Bismuth subsalicylate (Pepto-Bismol, others ®)
Drug Class: Colloidal Bismuth Compound
Mechanism of Action:
Like sucralfate, bismuth coats ulcers and erosions, creating a protective layer against acid and pepsin. It may also stimulate prostaglandins, mucus & bicarbonate secretion. It also has direct antimicrobial effects (e.g. against H. pylori) and binds enterotoxins (useful in treating traveler’s diarrhea). It also reduces stool frequency and liquidity in acute infectious diarrhea, due to salicylate inhibition of intestinal prostaglandins & chloride secretion.
Indications:
- treatment of dyspepsia &
- acute diarrhea,
- prevention of traveler’s diarrhea
Implication For Dentistry
Whether a patient is on a regimen of H2 blockers or antacids or has a history of gastric or duodenal ulcer, is important information for the dentist. Since this can influence the choice of a therapeutic agent or time of drug administration.
- The use of aspirin as an analgesic is contraindicated becauseof its irritating effect on gastric mucosa, esp in elderly patients.
- All NSAIDs share the ulcerogenic property of the salicylates – acetaminophen used as alternative analgesics as it produces minimal damage to gastric
- Systemic steroids if used after oral surgical procedures are potentially ulcerogenic.
- Even topical steroids used in the management of oral leisons should be avoided in the ulcer patients, because there absorption through the mucosa will occur.
- The choice of a preoperative or postoperative sedative is important for the ulcer patient. Chloral hydrate has irritating GIT side effects nausea & vomiting can occur.
- Diazepam is appropriate since in addition to producing sedation, it can suppress the nocturnal secretion of gastric acid.
- Absorption of orally administered diazepam is increased by the use of Al(OH)., Mg+ salt retards it absorption.
- For a patient being treated with cimetidine or omeprazole it is better to prescribe lorazepam or oxazepam, as antianxieity drugs, not depdendent on hepatic oxidative biotransformation. They are eliminated in the urine as glucuronide conjugates, the formation of which is not impaired by either cimetidine or omeprazole.
- Just one day of pretreatment with cimetidine causes much higher plasma concentrations of diazepam and a more pronounced sedative effect and slow elimination.
- Important in elderly patients, so diazepam if prescribed for a dental patient on cimetidine its dose should be reduced.
 howMed Know Yourself
howMed Know Yourself