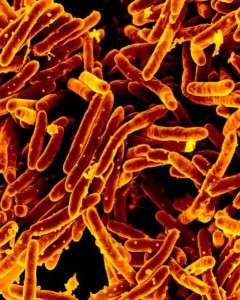
Mycobacterium tuberculosis is a non-motile, non-spore forming, non-encapsulated obligate aerobe. Under microscope, acid fast rods are observed.
Pathogenesis:
Transmission:
Person to person transmission occurs by respiratory aerosols. Aerosols are produced by coughing of smear positive people. Reactivation in elderly malnourished men is also seen.
Mycobacterium tuberculosis produces no exo or endotoxins. Bacteria infect macrophages and other reticuloendothelial cells. Bacteria survive and multiply in phagosomes. They release proteins called ‘exported and repetitive proteins’, which prevent fusion of phagosomes and lysosomes.
Bacteria cause two types of lesions depending upon organism and host response:
1. Exudative lesions: consisting of an acute inflammatory response and occur chiefly in lungs, in initial site of infection.
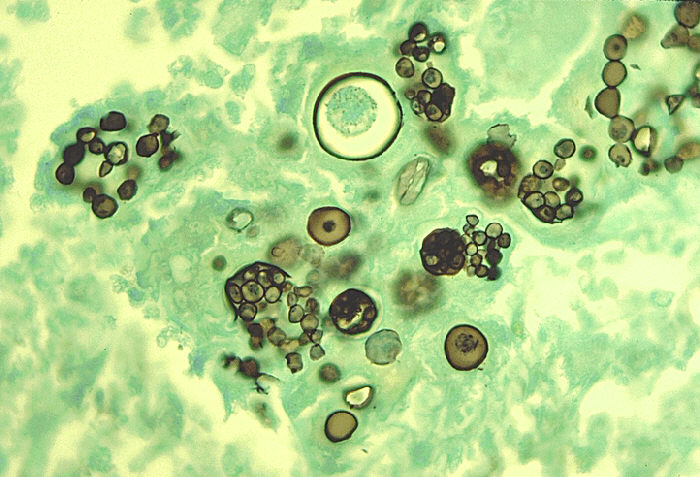
2. Granulomatous lesions: consisting of central area of giant cells, Langhan cells containing tubercle bacilli, surrounded by zone of epitheloid cells.
Tubercle is a granuloma surrounded by fibrous tissue that has undergone central caseation necrosis. Tubercles heal by fibrosis and calcification.
Primary lesions usually occur in lower lobes of lungs while reactivation lesions usually occur in apex of lungs and well oxygenated sites. Examples include kidneys, brain, bones, etc.
Bacteria spread in the body by two mechanisms :
1. A tubercles erodes into a bronchus, empties its contents and spreads the organism to other parts of lungs.
2. Through GIT if swallowed.
They disseminate via blood stream to other internal organs. Dissemination occurs at an early age if cell mediated immunity fails.
In its cell wall bacteria contain:
1. Mycolic acid: contributes to organism’s acid fastness.
2. Wax D, enhancement of antigen immunogenicity.
3. Phosphatides play role in caseous necrosis
4. Phthiocerol dimycocerosate is required for pathogenesis in lung
Virulence factors:
• Mycolic acids
• Wax D
• Phosphatides
• Phithiocerol dimycoceraste
• Exported repetitive protein
• Cord factors
Predisposing factors:
• Elderly malnourished men
• Poor housing
• Poor nutrition
Clinical symptoms:
• Cause tuberculosis
• Fever
• Fatigue
• Night sweats
• Weight loss
• Cough
• Hemoptysis
• Scrofula- mycobacterial cervical adenitis that presents as swollen non tender lymph nodes
• Erythrema nodosum
• Miliary tuberculosis characterized by multiple disseminted lesions
• Tuberculosis meningitis
• Tuberculosis osteomyelitis
Lab diagnosis:
Specimen:
• Sputum
• CSF- if tubercuosis meningitis is suspected
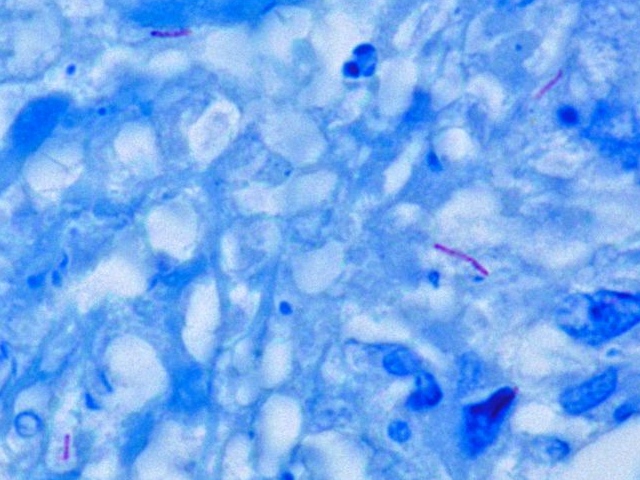
Microscopy:
• Acid fast rods
• Non-motile
• Non sporing
• Obligate aerobe
• Non capsulated
• Ziehl-neelson staining is used
Culture:
Grow slowly with doubling time of 18 hours.
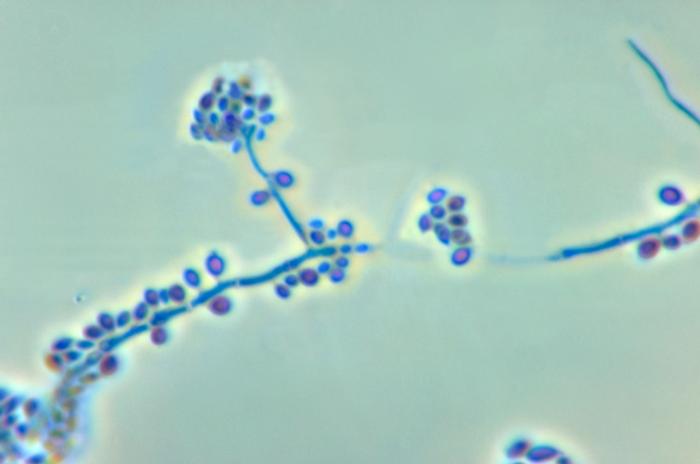
Virulent stains grow in a serpentine cord like pattern.
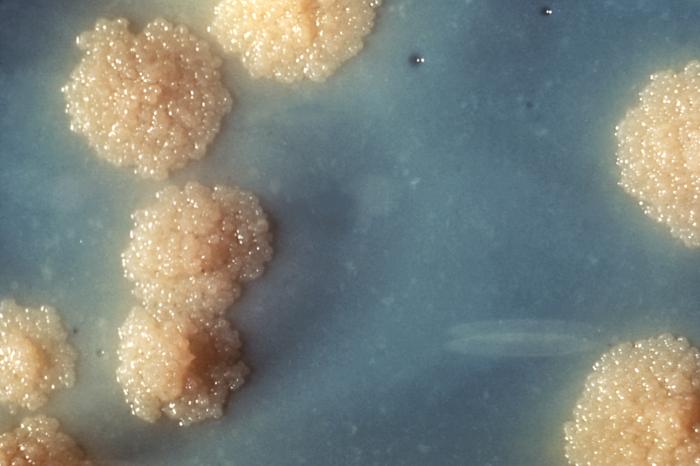
Lowenstenin Jensen agar
Raised, dry, cream colored colonies are visible after 2 to 3 weeks and sample is not discarded until 6 weeks of incubation.
Bactec medium
Nucleic acid amplification test
Luciferase assay
Luciferase produces flashes of light in presence of ATP.
Interferon gamma release assay
Quantiferon T.b
Biochemical tests:
Produce niacin and are catalase positive
Treatment:
• Isoniazid
• Rifampin
• Pyrazinamide
The three drugs are given for six months.
In disseminated disease, immunocompromised patients or isoniazid resistant strains, a fourth drug, ethambutol, is used and patient becomes non infectious within 2 to 3 weeks.
For multi-drug resistant strains, following drugs are applied:
i. Ciprofloxacin
ii. Amikacin
iii. Ethionamide
iv. Cycloserine
Reasons for Prolonged Therapy
• Intracellular location of organisms
• Caseous material blocks penetration by the drug
• Slow growth of the organism
• Metabolically inactive persisters within the lesion
 howMed Know Yourself
howMed Know Yourself